Anthem Claim Dispute Form With Provider In Travis
Description
Form popularity
FAQ
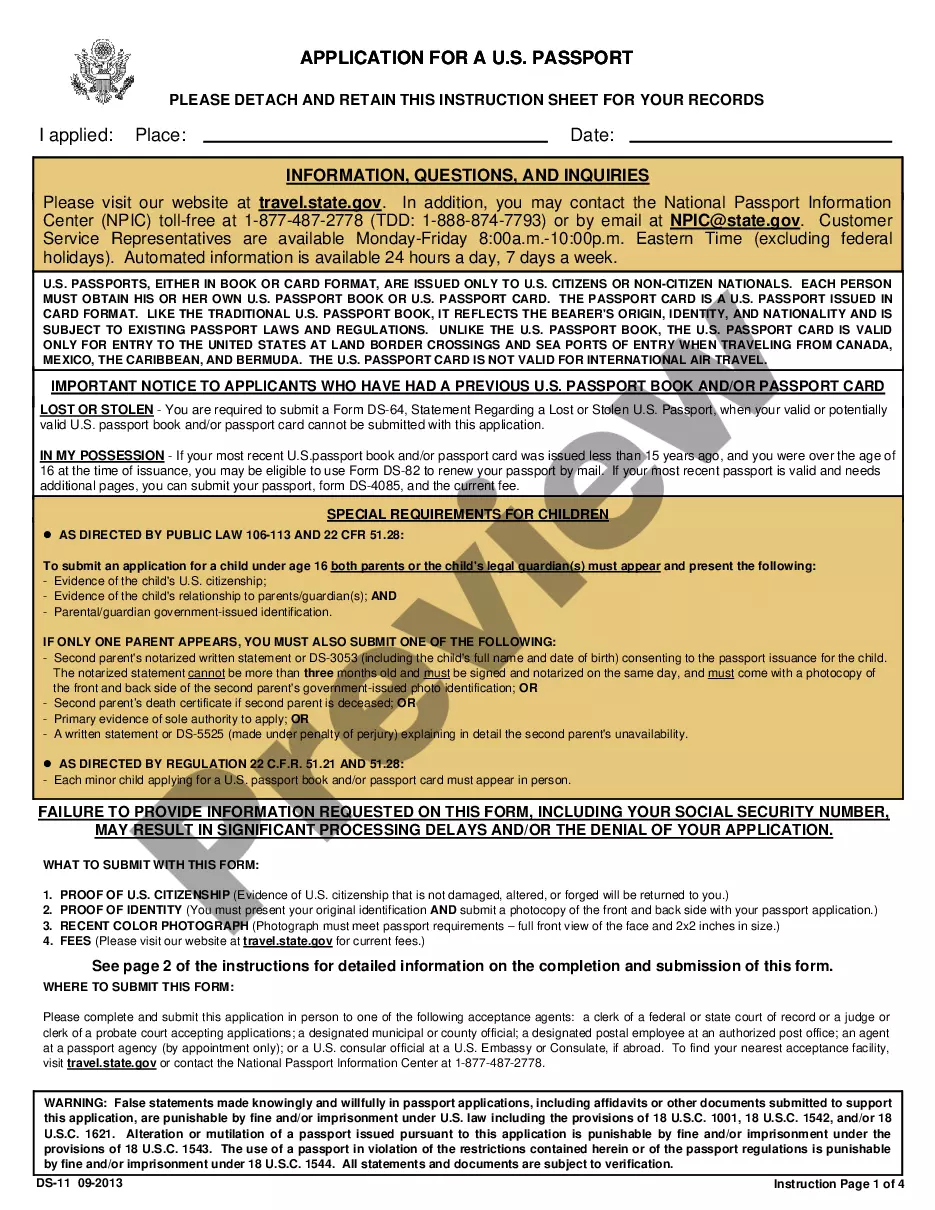
Things to Include in Your Appeal Letter Patient name, policy number, and policy holder name. Accurate contact information for patient and policy holder. Date of denial letter, specifics on what was denied, and cited reason for denial. Doctor or medical provider's name and contact information.
Case Management support is available 24/7 through Anthem Blue Cross Cal MediConnect Plan Customer Care at 1-855-817-5786.
To use the Appeals application, the Availity administrator must assign the Claim Status role for the user. The Disputes and Appeals functionality will support Appeals, Reconsiderations and Rework requests for providers. The Disputes and Appeals functionality is accessible from the Claim Status transaction.
A complaint (or grievance) – when you have a problem with Anthem or a provider, or with the healthcare or treatment you got from a provider. An appeal – when you don't agree with Anthem's decision to change your services or to not cover them.
Common Reasons Anthem Gives for Insurance Denials Reasons for Anthem insurance claims denials include: The filing deadline has expired. The insured mad a late payment to COBRA. The medical device or treatment sought is not medically necessary.
If your health plan has out-of-network benefits, we may reimburse you up to the maximum allowed amount for covered services if you see a non-participating provider.
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.
Send this claim to: Blue Shield of California, P.O. Box 272540, Chico, CA, 95927-2540.
The appeal must be received by Anthem Blue Cross (Anthem) within 365 days from the date on the notice of the letter advising of the action.
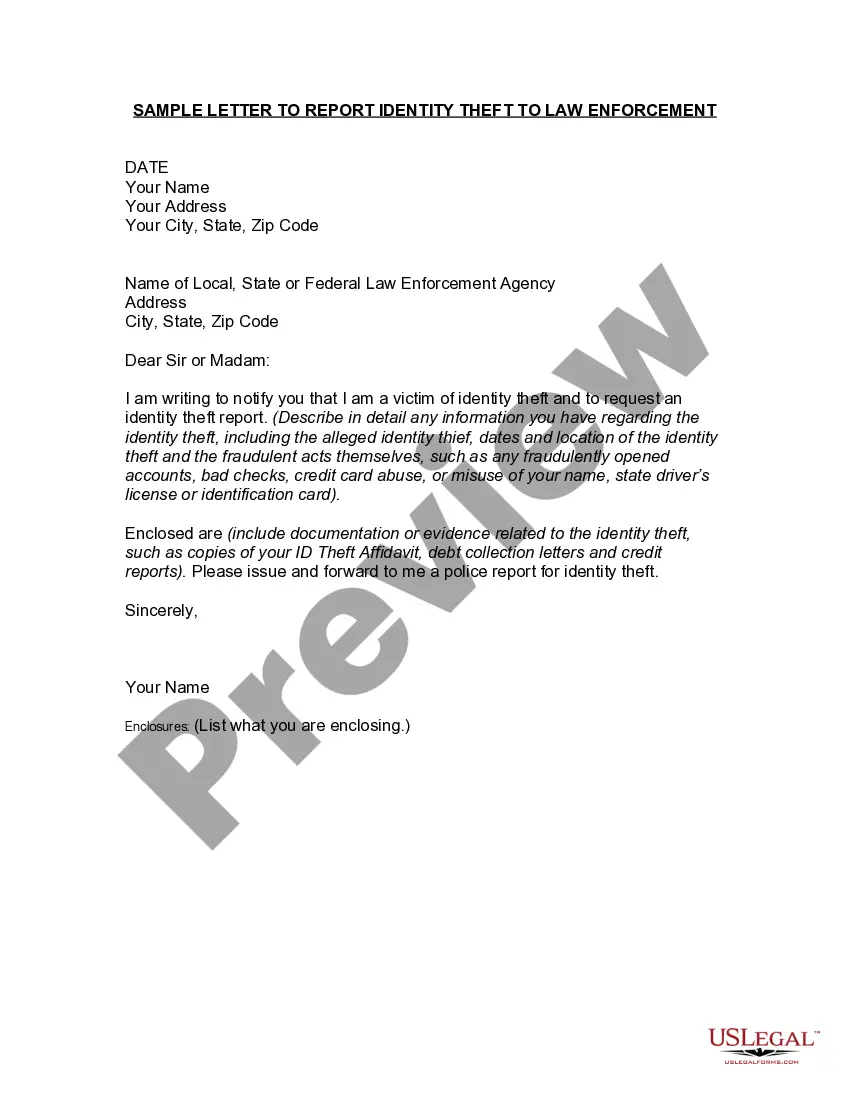
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form. This information is part of the permanent record. Write clearly and legibly.