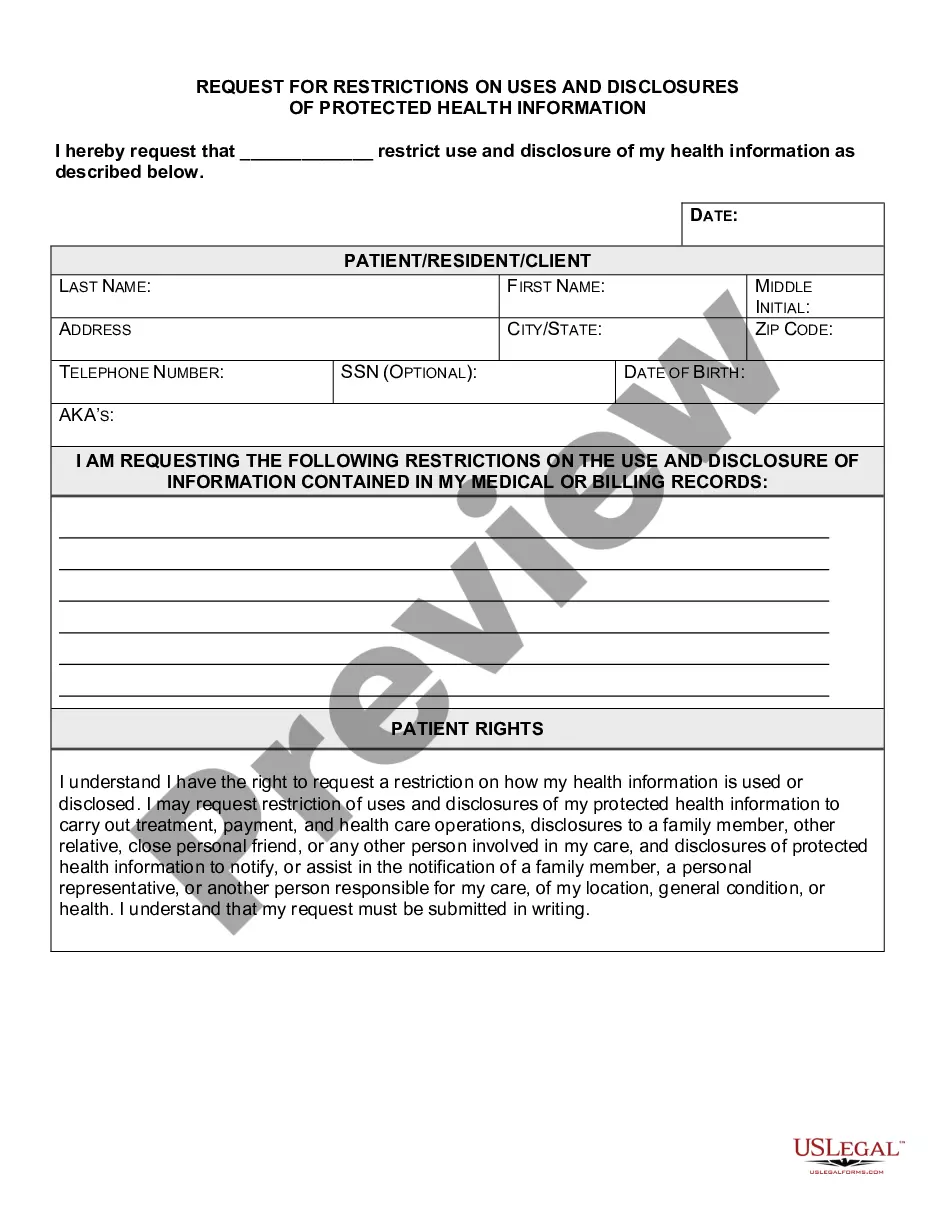
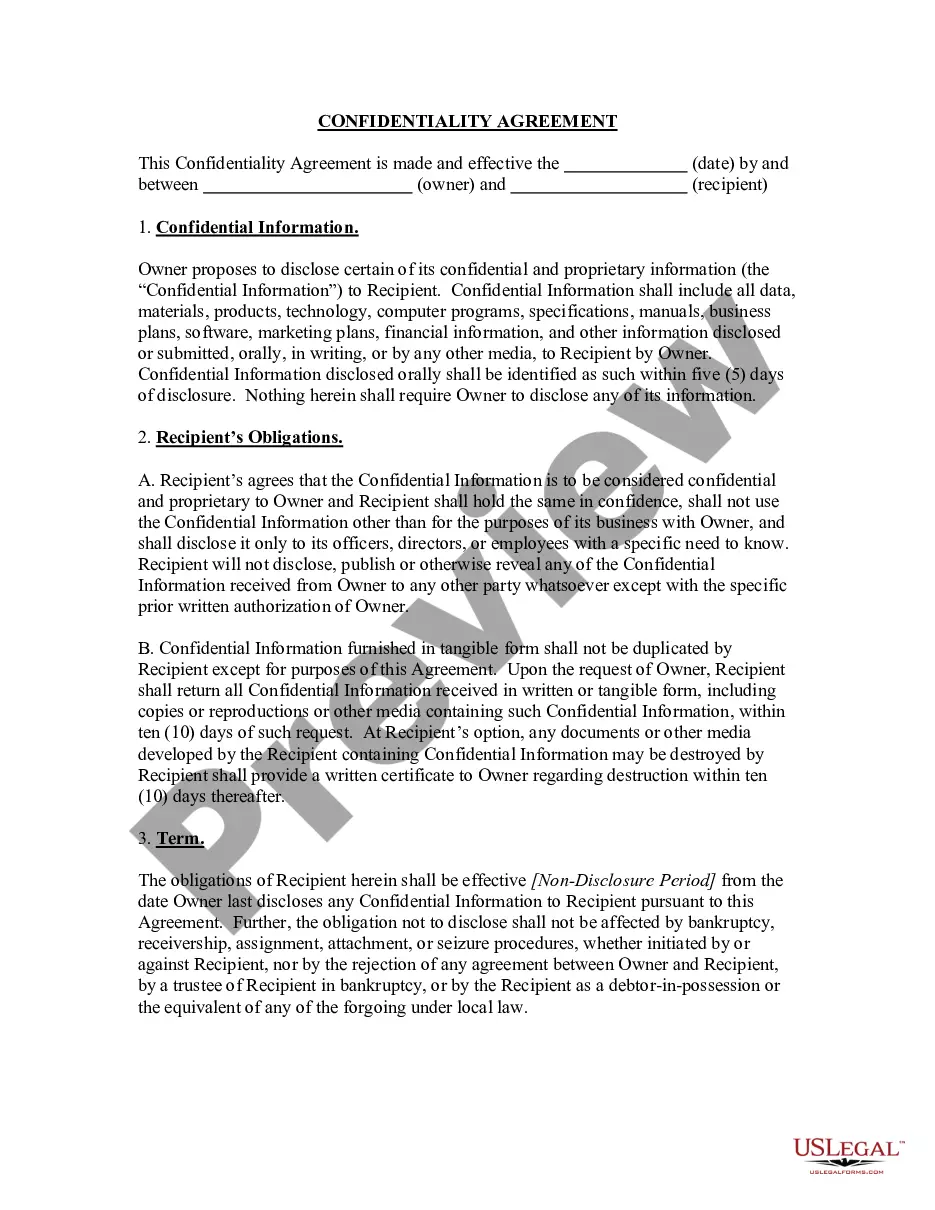
The Harris Texas Request for Restrictions on Uses and Disclosures of Protected Health Information is a crucial document that plays a significant role in safeguarding the privacy and security of individuals' healthcare information. This detailed description will provide an overview of the purpose, scope, and importance of this request, highlighting the key aspects and various types involved. The Harris Texas Request for Restrictions on Uses and Disclosures of Protected Health Information serves as a formal request made by an individual or their representative to impose restrictions on how their protected health information (PHI) is used and shared by healthcare entities. This request is based on the individual's right to privacy and aims to provide them with better control over their PHI. Under the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule, individuals have the right to request restrictions on the use or disclosure of their PHI. The Harris Texas Request for Restrictions form enables individuals to exercise this right and specify the limitations they prefer regarding the access, sharing, or usage of their healthcare information. This request is applicable to various entities within the healthcare domain, including healthcare providers, hospitals, clinics, pharmacies, health insurers, and any other covered entity under the HIPAA regulations. These entities are legally bound to comply with the individual's request unless an exception or an overriding requirement exists under the law. There can be different types of Harris Texas Request for Restrictions on Uses and Disclosures of Protected Health Information based on the specific limits an individual seeks to impose on their healthcare information. Some common scenarios include: 1. Restriction on Specific Healthcare Providers: Individuals may request restrictions on the release of their PHI to specific healthcare providers, allowing them to ensure their information is only shared with authorized professionals involved in their care. 2. Limitation on the Disclosure of Sensitive Information: Some individuals might want to restrict the disclosure of sensitive healthcare information like mental health records or substance abuse treatment details, ensuring that only relevant parties have access to such information. 3. Request for Non-Disclosure to Insurance Companies: Individuals might request restrictions on sharing their PHI with insurance companies for certain treatments or services they wish to keep confidential or pay out of pocket. 4. Exclusion of Specific Information from Electronic Health Record (EHR): Patients may ask for certain PHI details to be excluded or hidden within their electronic health record, ensuring that only authorized personnel can access or view this information. It is crucial for healthcare entities to respect and honor the restrictions imposed by an individual in their Request for Restrictions on Uses and Disclosures of Protected Health Information, as failure to comply can lead to serious legal consequences and violations of the individual's privacy rights. In conclusion, the Harris Texas Request for Restrictions on Uses and Disclosures of Protected Health Information empowers individuals to exercise their rights to privacy and control over their healthcare information. By submitting this request, individuals can define specific limitations on the use and sharing of their PHI, thereby ensuring their sensitive data remains secure and confidential throughout their healthcare journey.
Harris Texas Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
How to fill out Harris Texas Request For Restrictions On Uses And Disclosures Of Protected Health Information?
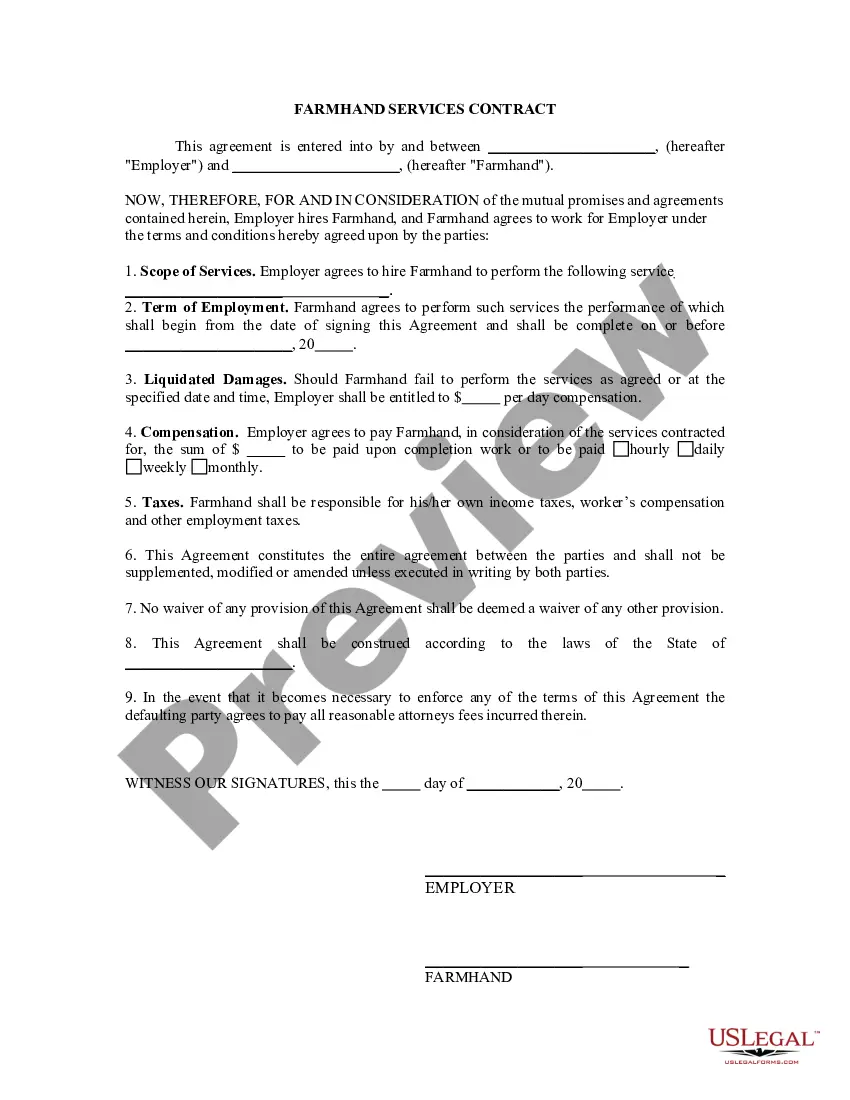
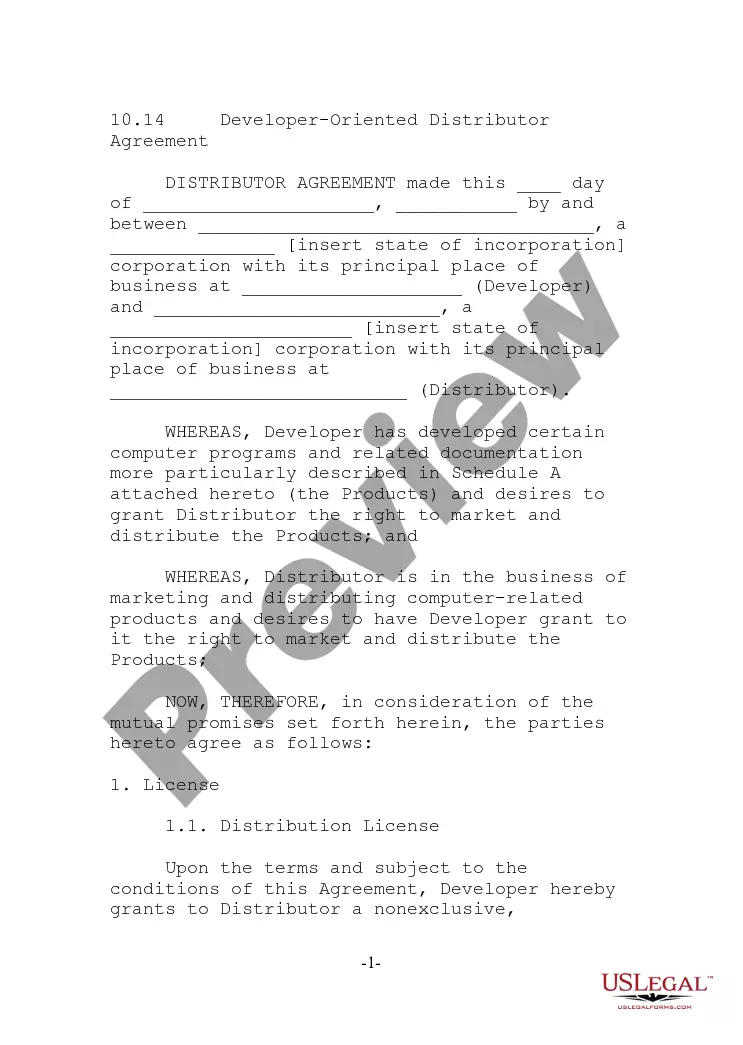
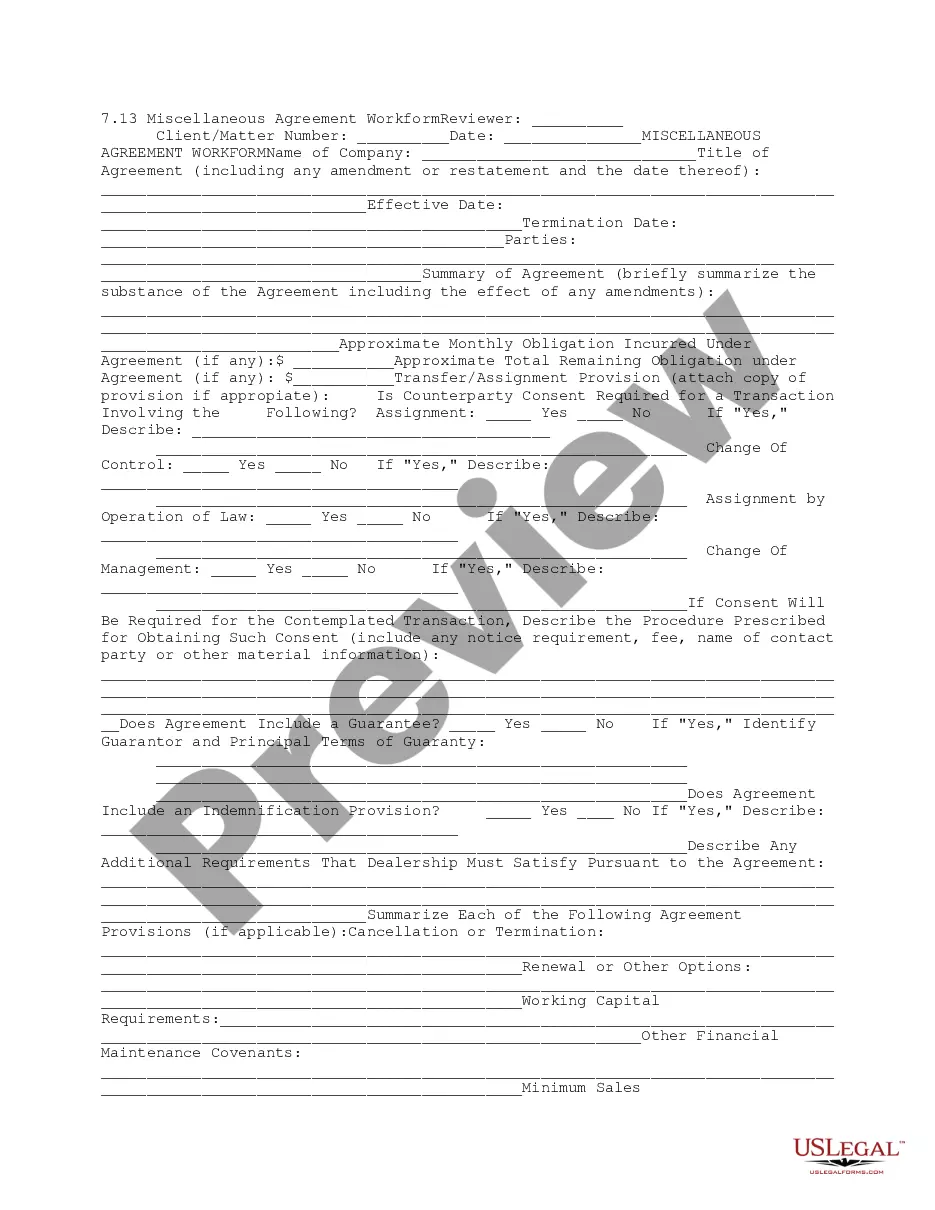
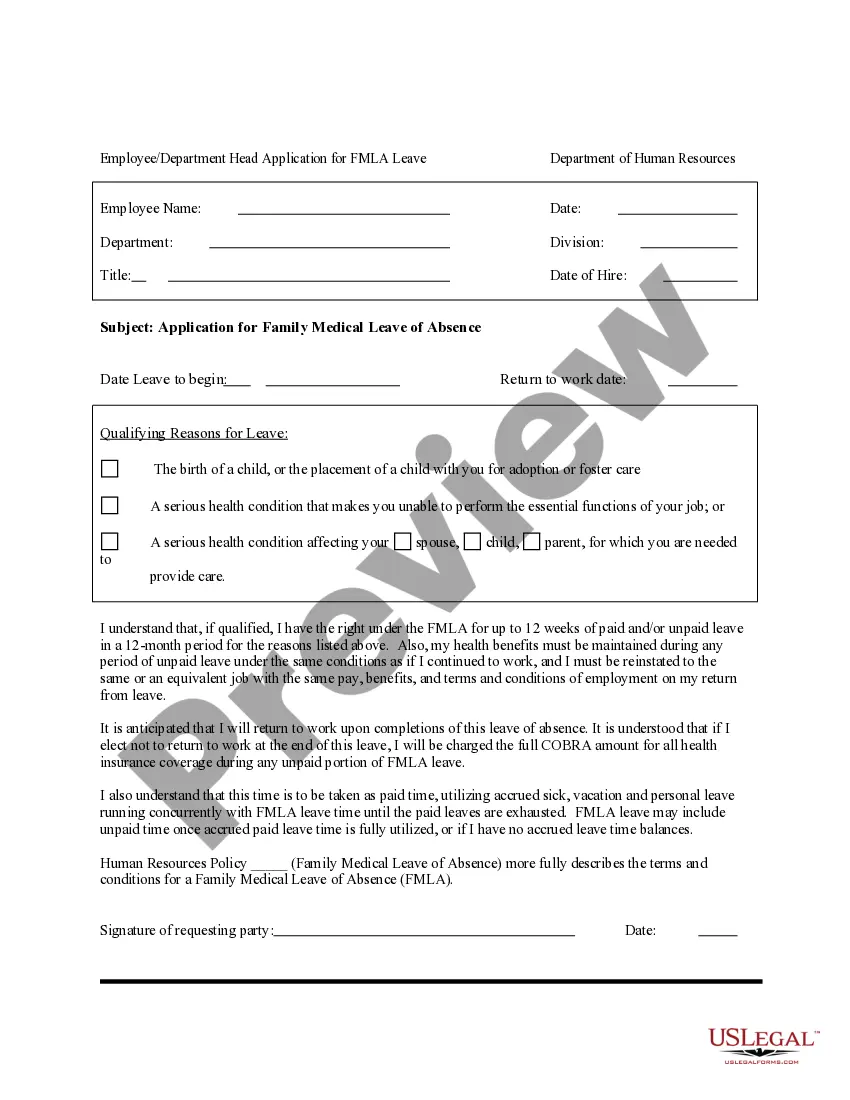
How much time does it normally take you to draft a legal document? Because every state has its laws and regulations for every life scenario, locating a Harris Request for Restrictions on Uses and Disclosures of Protected Health Information meeting all local requirements can be tiring, and ordering it from a professional attorney is often expensive. Numerous web services offer the most popular state-specific documents for download, but using the US Legal Forms library is most advantegeous.
US Legal Forms is the most comprehensive web collection of templates, gathered by states and areas of use. In addition to the Harris Request for Restrictions on Uses and Disclosures of Protected Health Information, here you can get any specific form to run your business or individual deeds, complying with your regional requirements. Professionals check all samples for their validity, so you can be sure to prepare your documentation properly.
Using the service is fairly easy. If you already have an account on the platform and your subscription is valid, you only need to log in, opt for the required form, and download it. You can retain the file in your profile at any time later on. Otherwise, if you are new to the website, there will be some extra steps to complete before you get your Harris Request for Restrictions on Uses and Disclosures of Protected Health Information:
- Check the content of the page you’re on.
- Read the description of the template or Preview it (if available).
- Look for another form using the related option in the header.
- Click Buy Now when you’re certain in the selected file.
- Choose the subscription plan that suits you most.
- Register for an account on the platform or log in to proceed to payment options.
- Pay via PalPal or with your credit card.
- Change the file format if necessary.
- Click Download to save the Harris Request for Restrictions on Uses and Disclosures of Protected Health Information.
- Print the sample or use any preferred online editor to complete it electronically.
No matter how many times you need to use the acquired document, you can find all the samples you’ve ever saved in your profile by opening the My Forms tab. Give it a try!
Form popularity
FAQ
Under HIPAA, PHI can be used and disclosed, without patient authorization, for essential healthcare operations, such as administrative, financial, legal, and quality improvement activities. Examples include: quality assessments for patient safety or general health/healthcare costs. in support of compliance.
A covered entity may disclose protected health information to the individual who is the subject of the information. (2) Treatment, Payment, Health Care Operations. A covered entity may use and disclose protected health information for its own treatment, payment, and health care operations activities.
Covered entities may disclose protected health information to: Public health authorities authorized by law to collect or receive such information for preventing or controlling disease, injury, or disability. Public health or other government authorities authorized to receive reports of child abuse and neglect.
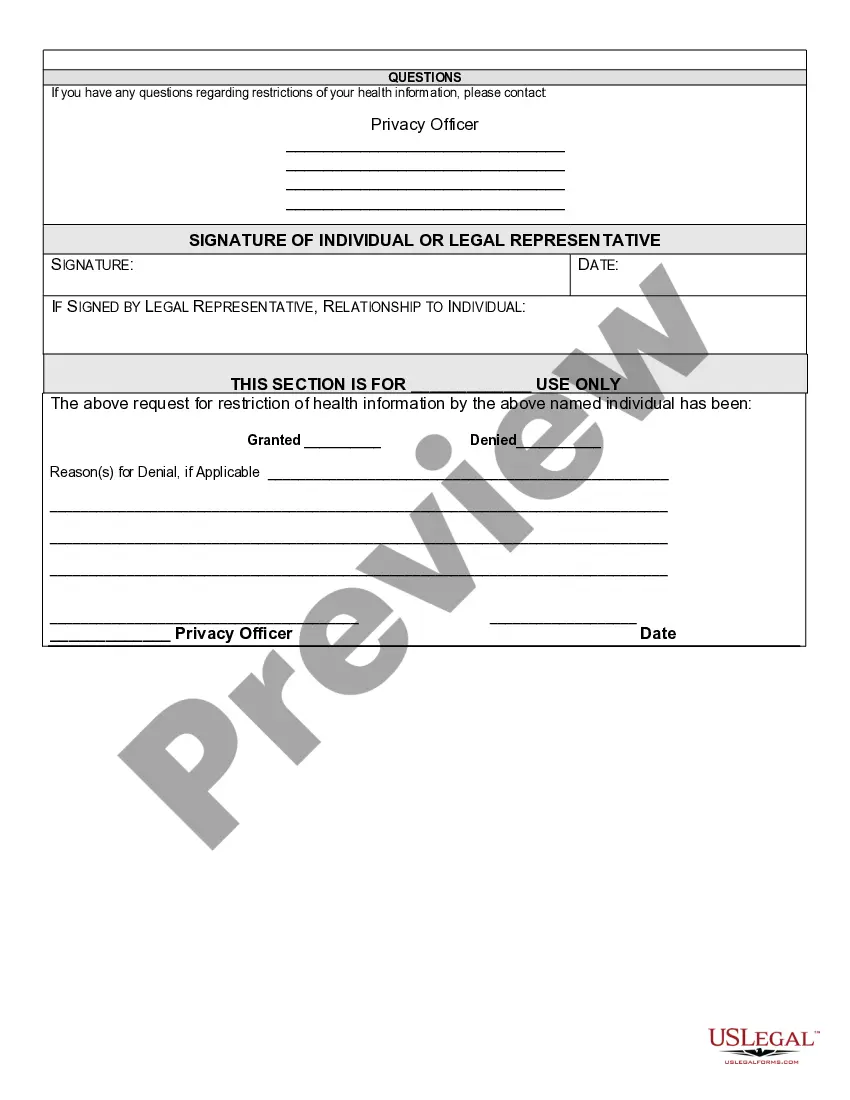
1. The right to request confidential communications and the process for making the request must be outlined in the Notice of Privacy Practices. 2. The patient, or patient's legal representative, shall complete and sign the Request for Confidential Communications form (see Attachment A).
You may disclose the PHI as long as you receive a request in writing. The written request must contain: the covered entity's name, the patient's name, the date of the event/time of treatment, and the reason for the request.
Required disclosure restriction: A facility must comply with a patient's request to restrict or limit the disclosure of the individual's protected health information (PHI) if 1) except as otherwise required by law, the disclosure is to a health plan for purposes of carrying out payment or health care operations (and is
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item
Note that an individual may not be required to provide a reason for requesting access, and the individual's rationale for requesting access, if voluntarily offered or known by the covered entity or business associate, is not a permitted reason to deny access.
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the
Restricted Disclosure is an alternative avenue for victims to report the occurrence of an incident of sexual misconduct and seek support, without automatically triggering a formal investigation.
Interesting Questions
More info
The patient authorizes termination. 6-12. The patient requests a waiver from this requirement. 13-15. We receive an order to restrict use of PHI to certain individuals, which we comply with. We will be obligated to restore your PHI to the extent that we have complied with the order. Furthermore, we cannot rescind an order to restrict your PHI. 18-22. Furthermore, we terminate PHI use and disclosure if: 1. The requested restriction is not followed. 2. The protected health information was disclosed in breach of any obligation under the law that relates to PHI use and disclosure. 3. We receive an order to restrict use, to be used exclusively by an authorized representative or a delegate of an authorized representative. 4. We receive an order to restrict the disclosurrion of protected health information, that we comply with. 5. This request is not permitted under HIPAA. 6. We notify your health plan that it is prohibited from allowing use or disclosure of PHI by the organization. 7.
Disclaimer
The materials in this section are taken from public sources. We disclaim all representations or any warranties, express or implied, as to the accuracy, authenticity, reliability, accessibility, adequacy, or completeness of any data in this paragraph. Nevertheless, we make every effort to cite public sources deemed reliable and trustworthy.