Arvada Colorado Request for Utilization Review for Workers' Compensation is a necessary procedure for individuals seeking workers' compensation benefits in Arvada, Colorado, related to work-related injuries or illnesses. This request aims to ensure that the medical treatments and services provided to the injured employee are reasonable, necessary, and appropriate for their specific condition, while also conforming to the guidelines and regulations of the workers' compensation system. Workers' compensation is a form of insurance that provides wage replacement and medical benefits to employees who have been injured or become ill in the course of their job duties. In Arvada, Colorado, employers are obligated to provide these benefits to their employees and comply with the rules and regulations set by the state. When an employee sustains a work-related injury or illness, they are entitled to receive appropriate medical care to aid in their recovery. However, there are instances where the necessity and appropriateness of certain treatments or services may come into question. In such cases, the Arvada Colorado Request for Utilization Review for Workers' Compensation is initiated. The Utilization Review process involves the careful assessment of the medical treatment plan proposed by the treating healthcare provider. This review assesses whether the procedures, therapies, medications, or surgeries recommended are the most effective and suitable options for the injured employee's condition. The goal is to ensure that the worker receives optimal care while preventing unnecessary or excessive medical expenses. Upon filing the Arvada Colorado Request for Utilization Review for Workers' Compensation, the injured employee's case is reviewed by a team of qualified medical professionals who specialize in workers' compensation. Based on their expertise and understanding of the applicable guidelines, they assess the medical documentation and make a determination regarding the appropriateness of the proposed treatment plan. Different types of Arvada Colorado Request for Utilization Review for Workers' Compensation may include specific variations based on the nature of the injury or illness, such as: 1. Physical Therapy Request for Utilization Review for Workers' Compensation: This focuses on the evaluation of the necessity and effectiveness of physical therapy treatments prescribed for an injured employee's rehabilitation. 2. Surgical Procedure Request for Utilization Review for Workers' Compensation: This type of review concentrates on assessing the necessity and appropriateness of a proposed surgical intervention for the work-related injury or illness. 3. Medication Request for Utilization Review for Workers' Compensation: This particular review involves a detailed evaluation of the medications prescribed to the injured employee, determining their suitability according to the guidelines and assessing if alternative treatments could have been considered. By conducting a thorough Arvada Colorado Request for Utilization Review for Workers' Compensation, employers and insurers can ensure that workers' compensation benefits are used effectively and in adherence to the established protocols, resulting in optimal care for injured employees while ensuring cost-efficiency.
Arvada Colorado Request for Utilization Review for Workers' Compensation
Description
How to fill out Arvada Colorado Request For Utilization Review For Workers' Compensation?
Finding verified templates specific to your local regulations can be challenging unless you use the US Legal Forms library. It’s an online pool of more than 85,000 legal forms for both personal and professional needs and any real-life situations. All the documents are properly grouped by area of usage and jurisdiction areas, so locating the Arvada Colorado Request for Utilization Review for Workers' Compensation becomes as quick and easy as ABC.
For everyone already familiar with our catalogue and has used it before, getting the Arvada Colorado Request for Utilization Review for Workers' Compensation takes just a few clicks. All you need to do is log in to your account, select the document, and click Download to save it on your device. This process will take just a couple of additional steps to complete for new users.
Follow the guidelines below to get started with the most extensive online form catalogue:
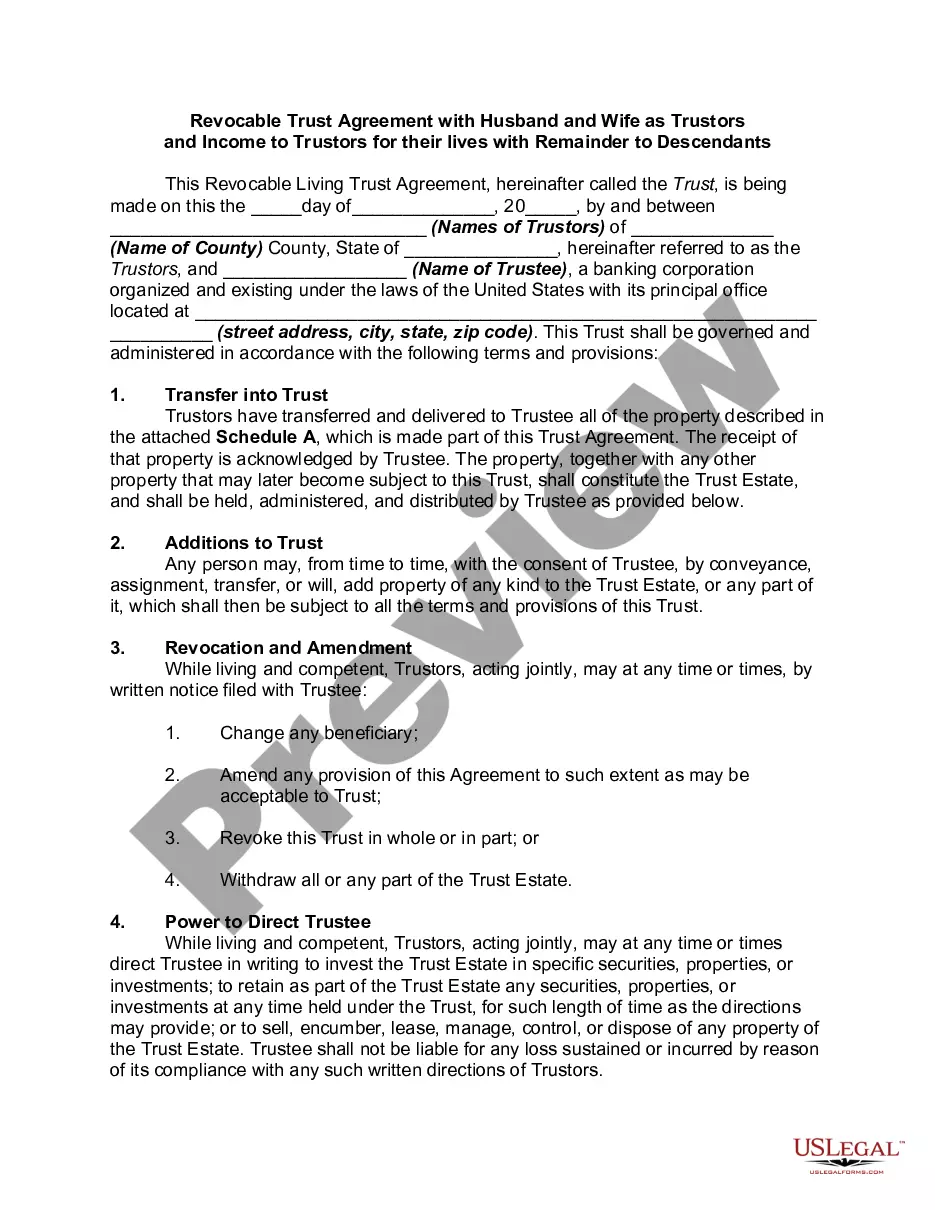
- Look at the Preview mode and form description. Make sure you’ve chosen the right one that meets your requirements and totally corresponds to your local jurisdiction requirements.
- Look for another template, if needed. Once you see any inconsistency, utilize the Search tab above to get the right one. If it suits you, move to the next step.
- Buy the document. Click on the Buy Now button and choose the subscription plan you prefer. You should sign up for an account to get access to the library’s resources.
- Make your purchase. Give your credit card details or use your PayPal account to pay for the subscription.
- Download the Arvada Colorado Request for Utilization Review for Workers' Compensation. Save the template on your device to proceed with its completion and obtain access to it in the My Forms menu of your profile anytime you need it again.
Keeping paperwork neat and compliant with the law requirements has significant importance. Take advantage of the US Legal Forms library to always have essential document templates for any demands just at your hand!
Form popularity
FAQ
In California, all employers or insurance companies handling workers' compensation claims are required to have a utilization review (UR) program. A UR program allows an employer or insurance company to review a treatment request made by an injured worker's physician to determine if the treatment is medically necessary.
The decision on an RFA submitted for prospective review must be made within five business days from first receipt of the request, unless additional reasonable medical information is needed to make the decision.
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
(o) A utilization review decision to modify, delay, or deny a request for authorization of medical treatment shall remain effective for 12 months from the date of the decision without further action by the claims administrator with regard to any further recommendation by the same physician for the same treatment unless
The claims administrator must do the review and make a decision within five days of the date your doctor requested the treatment. If additional information is needed to make a decision, the claims administrator can have up to 14 days. Q.
Utilization review is a method used to match the patient's clinical picture and care interventions to evidence-based criteria such as MCG care guidelines. This criteria helps to guide the utilization review nurse in determining the appropriate care setting for all levels of services across the arc of patient care.
(o) A utilization review decision to modify, delay, or deny a request for authorization of medical treatment shall remain effective for 12 months from the date of the decision without further action by the claims administrator with regard to any further recommendation by the same physician for the same treatment unless
An Example of Utilization Review Sam is admitted to the ICU through the emergency room in the middle of the night after a car accident. The next morning, the hospital's UR nurse looks at Sam's medical record and notes all of his medical problems and treatments.
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
1. What is Utilization Review? Utilization review is the approval, modification, or denial of the medical treatment recommended by the injured worker's doctor. 1. Medical treatment is one of the benefits an injured worker receives in the California workers' compensation system.