Wisconsin Sample COBRA Enrollment and / or Waiver Letter
Description
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
If you need to obtain extensive, download, or print official document templates, utilize US Legal Forms, the premier collection of legal templates, accessible online.
Employ the website's simple and convenient search function to find the documents you require.
A variety of templates for commercial and personal purposes are organized by categories and states, or keywords.
Step 3. If you are not satisfied with the form, use the Search field at the top of the screen to find alternative versions of the legal form template.
Step 4. After locating the form you need, click the Purchase Now button. Select the payment plan you prefer and enter your details to register for an account.
- Utilize US Legal Forms to acquire the Wisconsin Sample COBRA Enrollment and/or Waiver Letter with just a few clicks.
- If you are already a US Legal Forms member, Log In to your account and click the Order button to find the Wisconsin Sample COBRA Enrollment and/or Waiver Letter.
- You can also view templates you previously downloaded in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the guidelines outlined below.
- Step 1. Ensure you have chosen the form for your correct city/state.
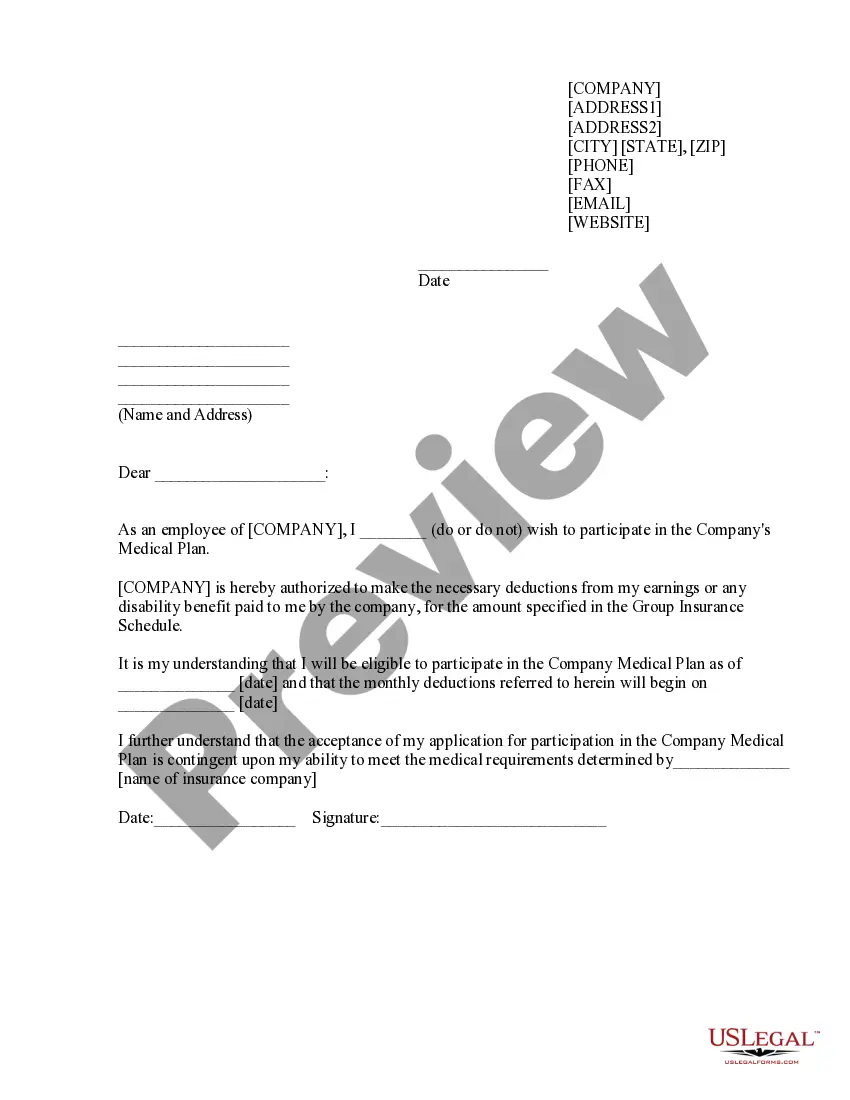
- Step 2. Use the Preview option to review the form's content. Don’t forget to read the details.
Form popularity
FAQ
The purpose of this letter is to inform you of your rights and responsibilities as a plan participant. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a landmark federal law, passed in 1985, that provides for continuing group health insurance coverage for some employees and their families after a job loss or other qualifying event.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
Failure to pay premiums. When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
Federal Law (COBRA) Under federal law, employees who have a reduction in work hours or terminate employment for any reason other than gross misconduct may continue their group coverage for up to 18 months. (A spouse and dependents are also covered.)