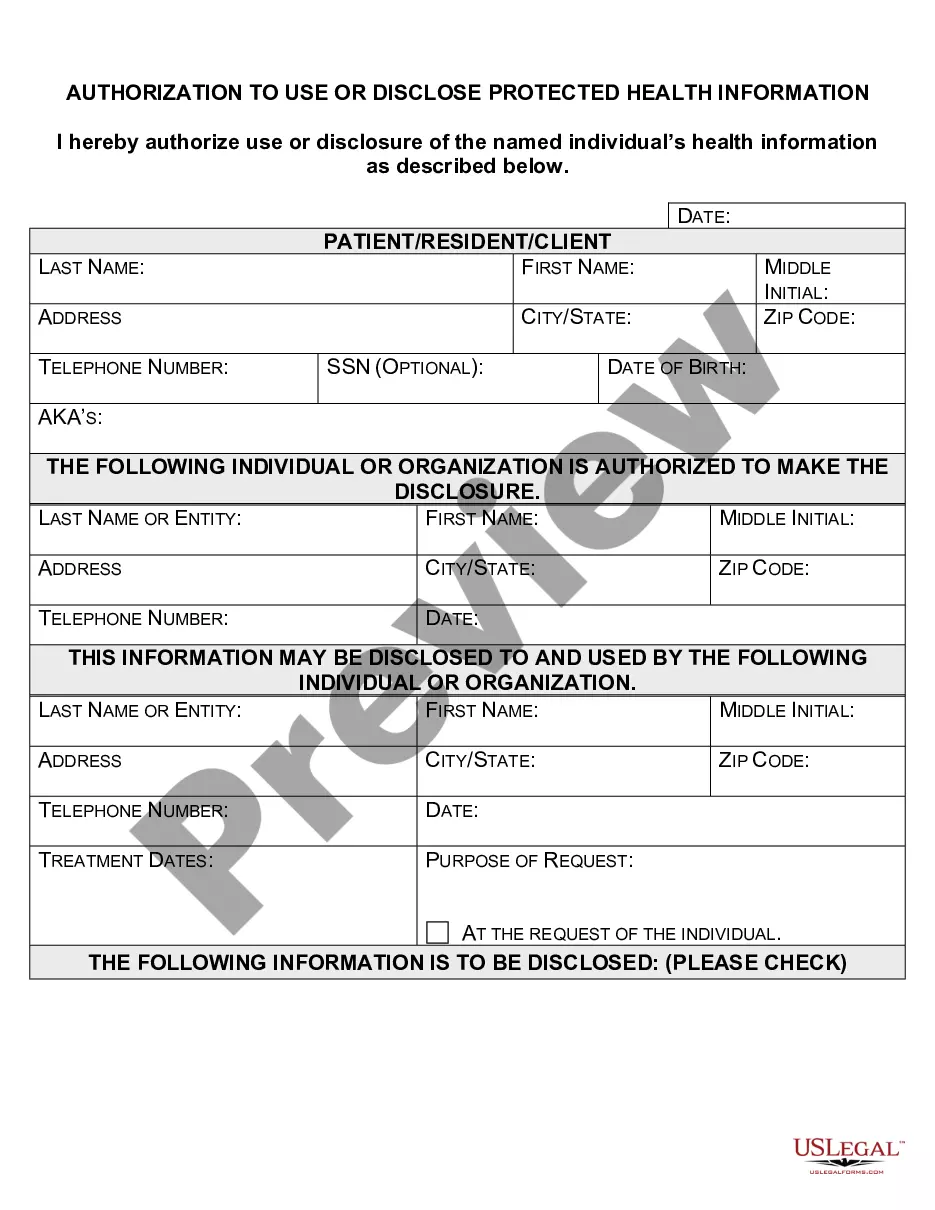
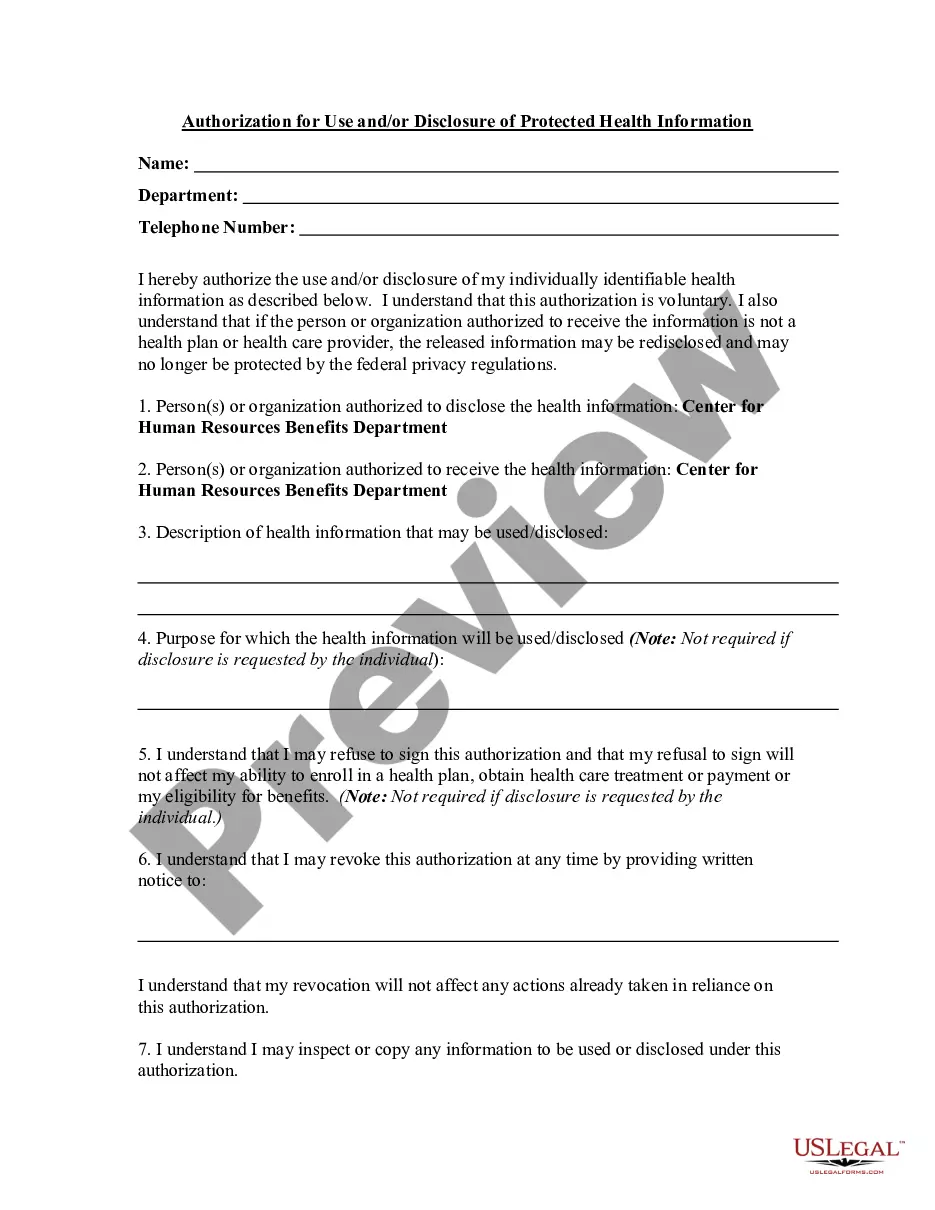
Vermont Authorization to Use or Disclose Protected Health Information
Description
How to fill out Authorization To Use Or Disclose Protected Health Information?
Are you currently situated in an environment where you need paperwork for either professional or personal purposes almost every day.
There are numerous legal document templates accessible online, but finding reliable ones can be challenging.
US Legal Forms provides thousands of form templates, including the Vermont Authorization to Use or Disclose Protected Health Information, designed to meet state and federal requirements.
Once you locate the appropriate form, click Acquire now.
Choose the pricing plan you desire, fill out the required information to create your account, and pay for the transaction using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- After logging in, you can download the Vermont Authorization to Use or Disclose Protected Health Information template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Find the form you need and ensure it is for the correct city/area.
- Utilize the Review option to examine the document.
- Check the description to confirm that you’ve selected the correct form.
- If the form is not what you are looking for, use the Lookup section to find a form that suits your needs.
Form popularity
FAQ
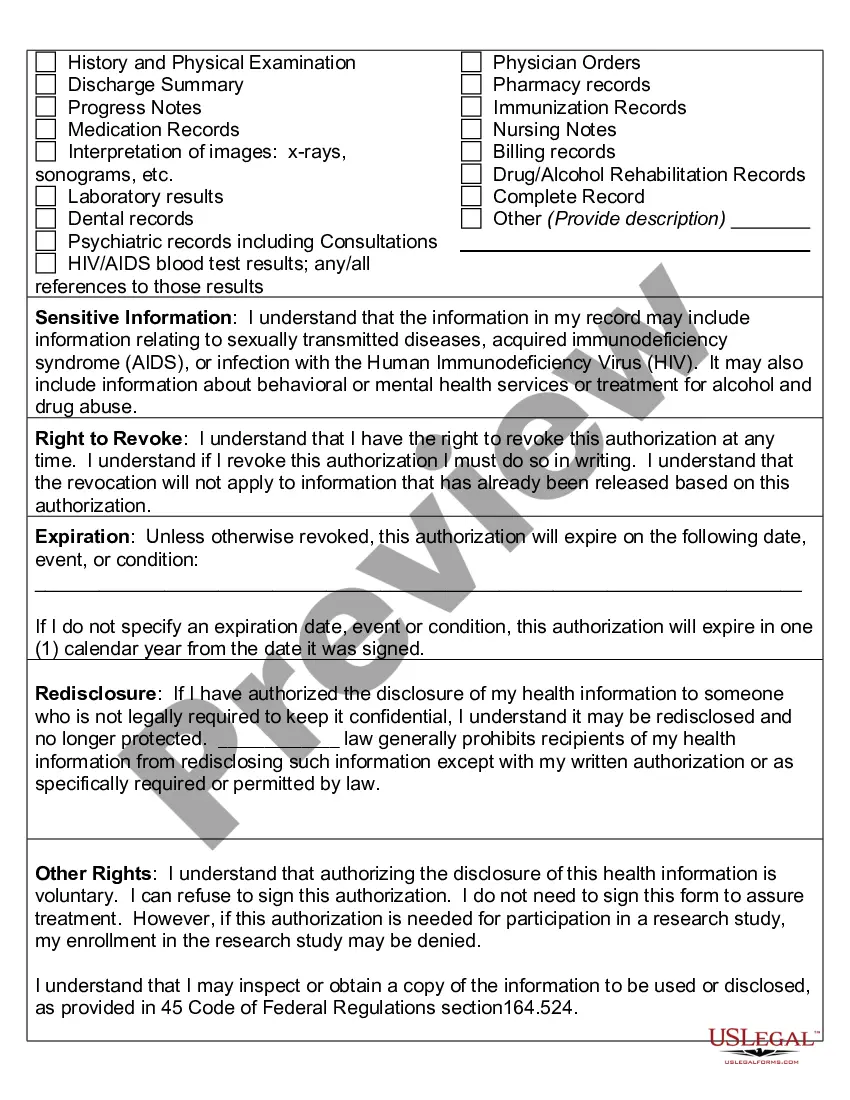
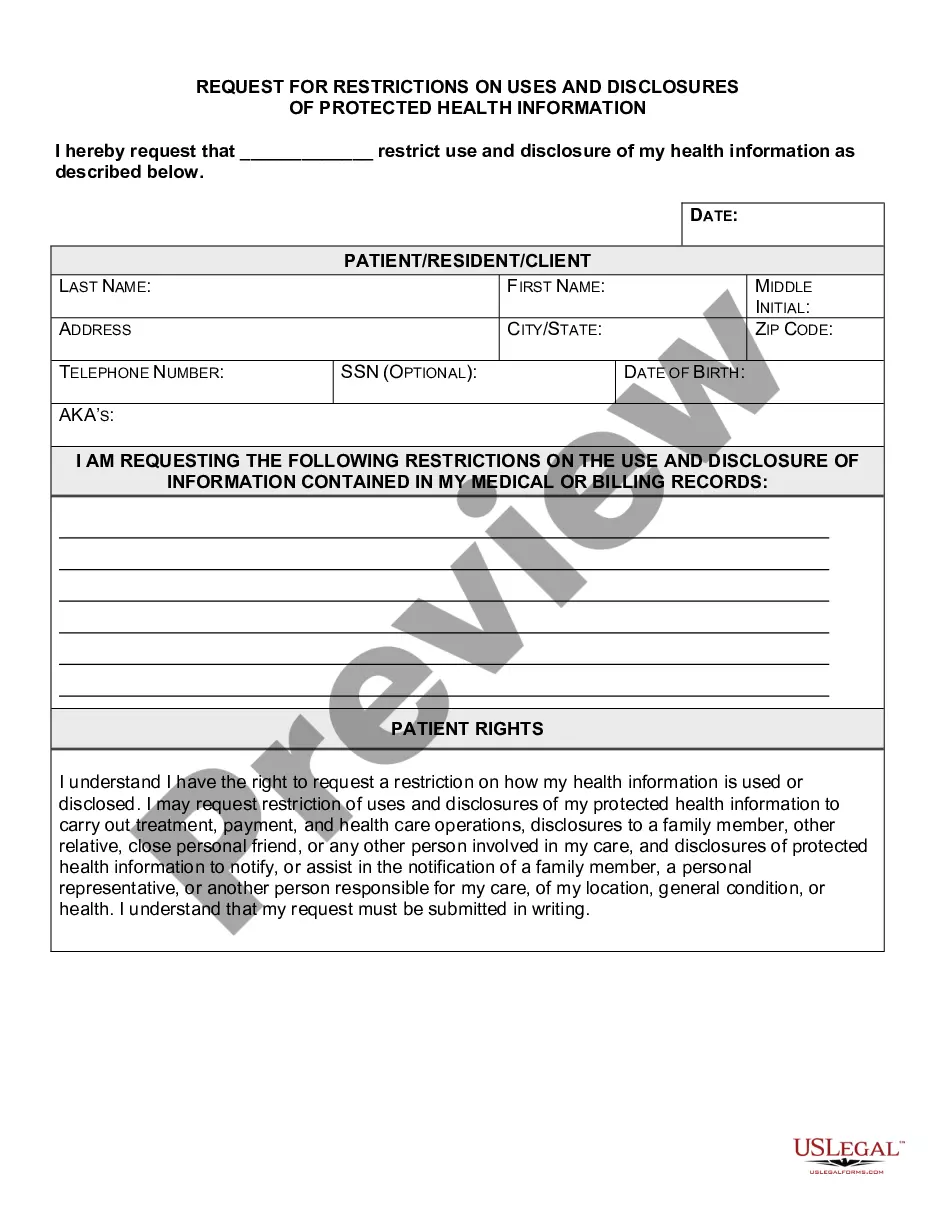
A covered entity may disclose private health information without authorization in certain circumstances defined by HIPAA. These include disclosures for treatment, payment, and healthcare operations, as well as in emergencies or as required by law. Understanding when and how this applies can help you navigate privacy concerns. The complexities around the Vermont Authorization to Use or Disclose Protected Health Information can be better managed with resources available on platforms like USLegalForms.
A patient authorization is not required for disclosure of PHI between Covered Entities if the disclosure is needed for purposes of treatment or payment or for healthcare operations. You may disclose the PHI as long as you receive a request in writing.
Health information such as diagnoses, treatment information, medical test results, and prescription information are considered protected health information under HIPAA, as are national identification numbers and demographic information such as birth dates, gender, ethnicity, and contact and emergency contact
A violation is an unauthorized disclosure that results in the conclusion there is a low probability of compromise to the PHI. If this low risk is determined and supported by the Risk Assessment, reporting the incident to the OCR and the involved patient is deemed to be unnecessary.
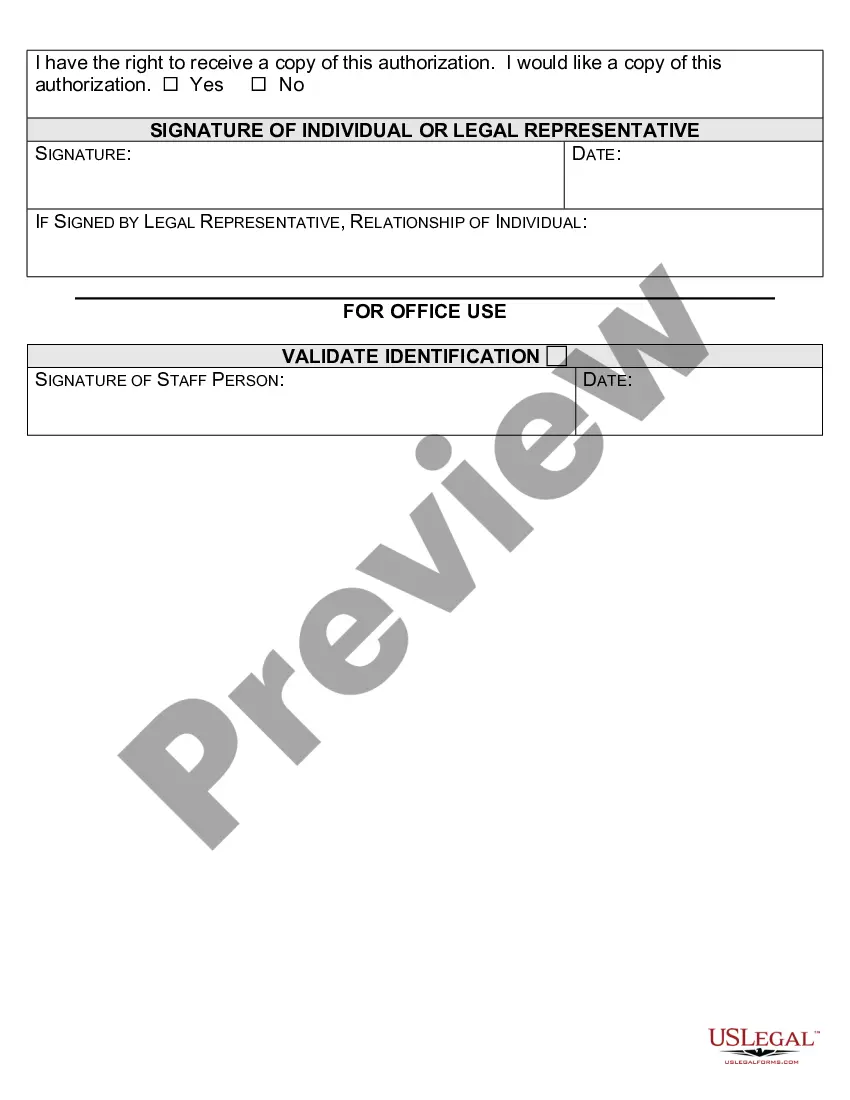
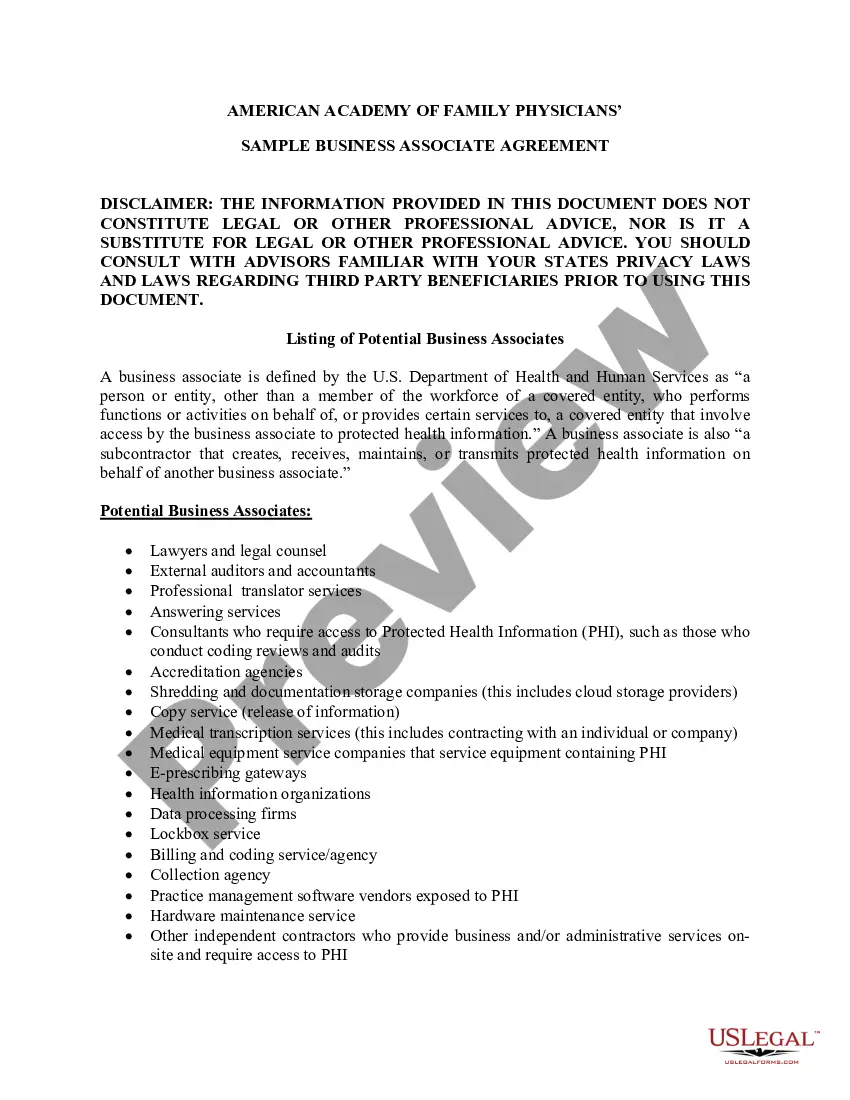
Valid HIPAA Authorizations: A ChecklistNo Compound Authorizations. The authorization may not be combined with any other document such as a consent for treatment.Core Elements.Required Statements.Marketing or Sale of PHI.Completed in Full.Written in Plain Language.Give the Patient a Copy.Retain the Authorization.
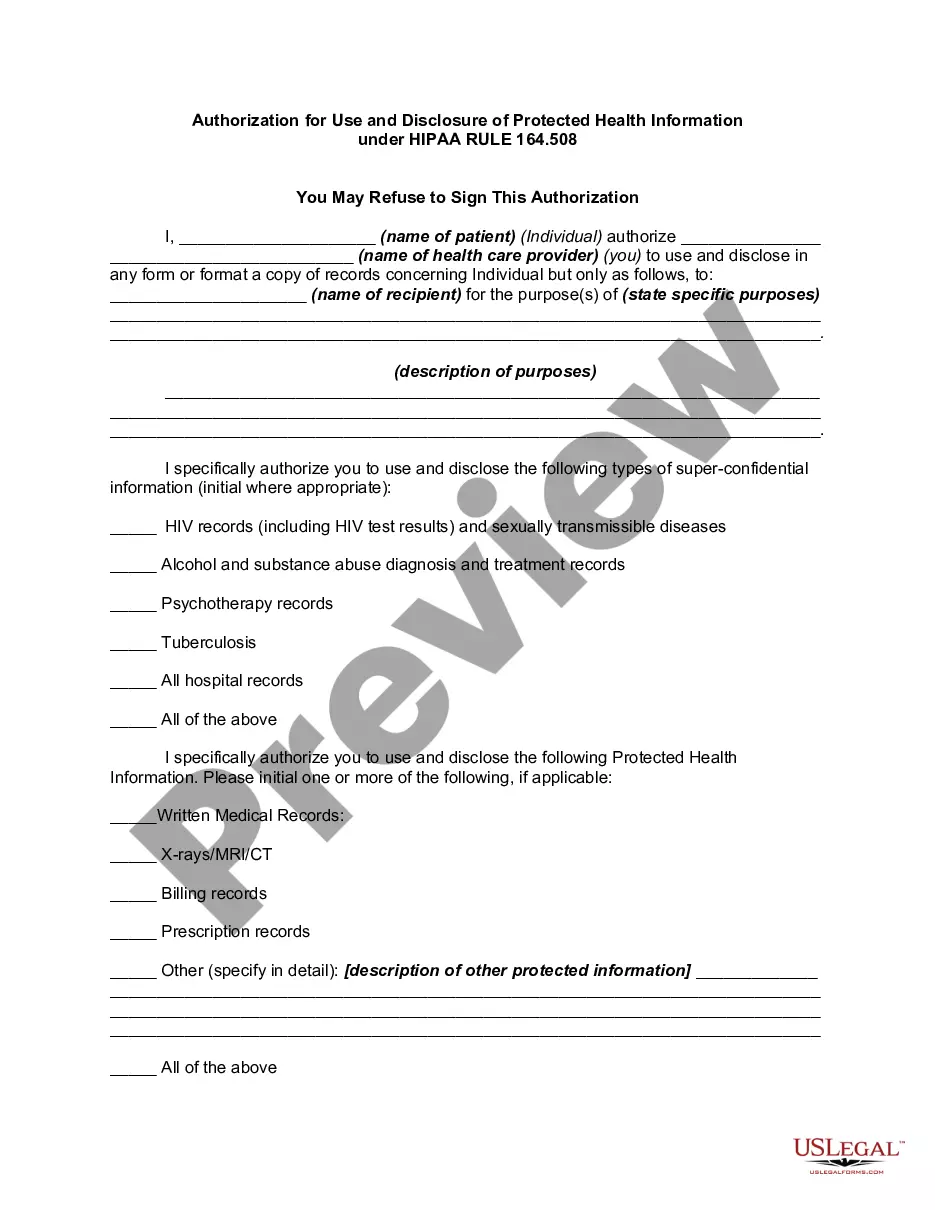
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the
A HIPAA authorization is a detailed document in which specific uses and disclosures of protected health are explained in full. By signing the authorization, an individual is giving consent to have their health information used or disclosed for the reasons stated on the authorization.
Under the HIPAA Privacy Rule, a covered entity must disclose protected health information in only two situations: (a) to individuals (or their personal representatives) specifically when they request access to, or an accounting of disclosures of, their protected health information; and (b) to the Department of Health
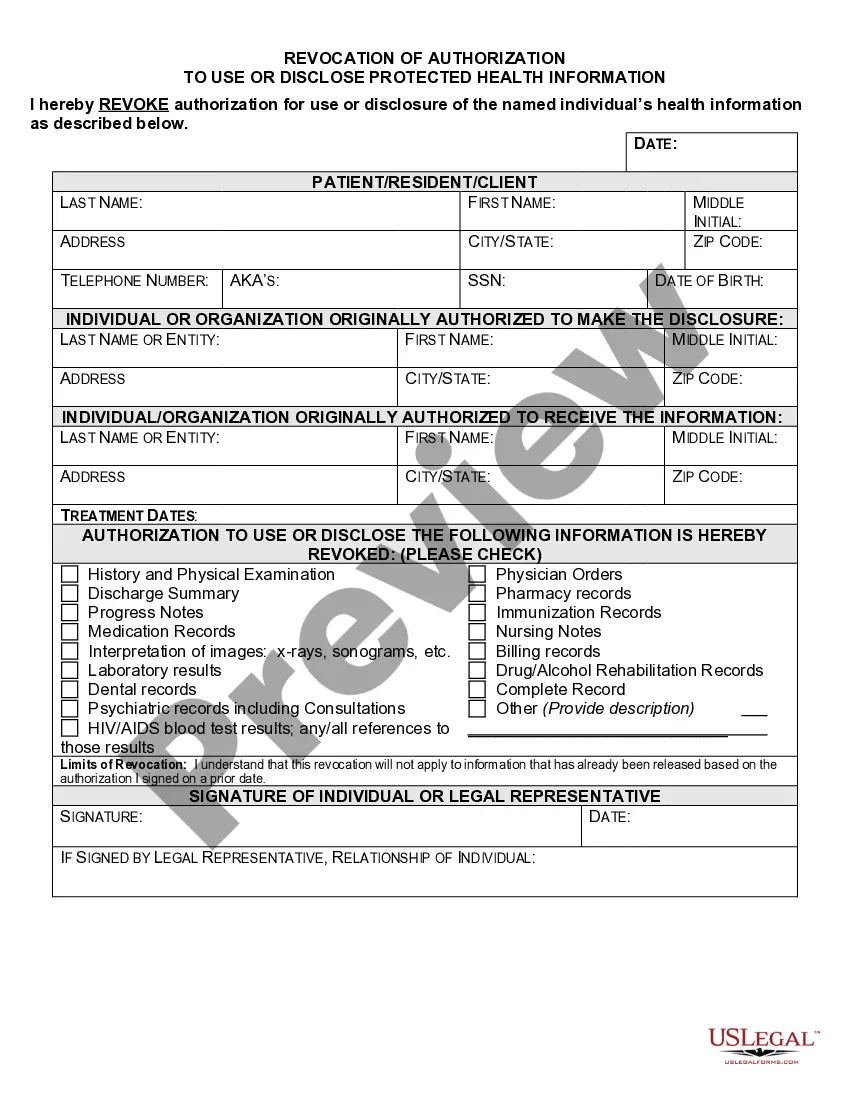
What are two required elements of an authorization needed to disclose PHI? Response Feedback: All authorizations to disclose PHI must have an expiration date and provide an avenue for the patient to revoke his or her authorization. What does the term "Disclosure" mean?
A breach is, generally, an impermissible use or disclosure under the Privacy Rule that compromises the security or privacy of the protected health information.