Virginia Notice of Special Enrollment Rights
Description
How to fill out Notice Of Special Enrollment Rights?
US Legal Forms - one of several biggest libraries of legal forms in the States - delivers an array of legal document themes you are able to acquire or produce. Utilizing the web site, you can find a large number of forms for business and specific uses, sorted by classes, claims, or search phrases.You can get the most up-to-date models of forms like the Virginia Notice of Special Enrollment Rights within minutes.
If you currently have a registration, log in and acquire Virginia Notice of Special Enrollment Rights from your US Legal Forms library. The Acquire key will appear on every type you see. You have accessibility to all earlier delivered electronically forms inside the My Forms tab of your account.
If you would like use US Legal Forms for the first time, listed here are straightforward recommendations to help you get started:
- Make sure you have chosen the best type for your area/region. Click the Preview key to analyze the form`s content. See the type explanation to ensure that you have chosen the appropriate type.
- When the type does not fit your needs, take advantage of the Search field on top of the screen to discover the one that does.
- When you are content with the form, validate your decision by visiting the Purchase now key. Then, pick the rates prepare you like and offer your references to sign up on an account.
- Approach the financial transaction. Make use of Visa or Mastercard or PayPal account to accomplish the financial transaction.
- Choose the formatting and acquire the form on the system.
- Make modifications. Complete, modify and produce and indicator the delivered electronically Virginia Notice of Special Enrollment Rights.
Every single template you added to your bank account does not have an expiration date which is the one you have for a long time. So, in order to acquire or produce yet another duplicate, just check out the My Forms section and click around the type you require.
Obtain access to the Virginia Notice of Special Enrollment Rights with US Legal Forms, one of the most substantial library of legal document themes. Use a large number of specialist and state-particular themes that meet up with your organization or specific demands and needs.
Form popularity
FAQ
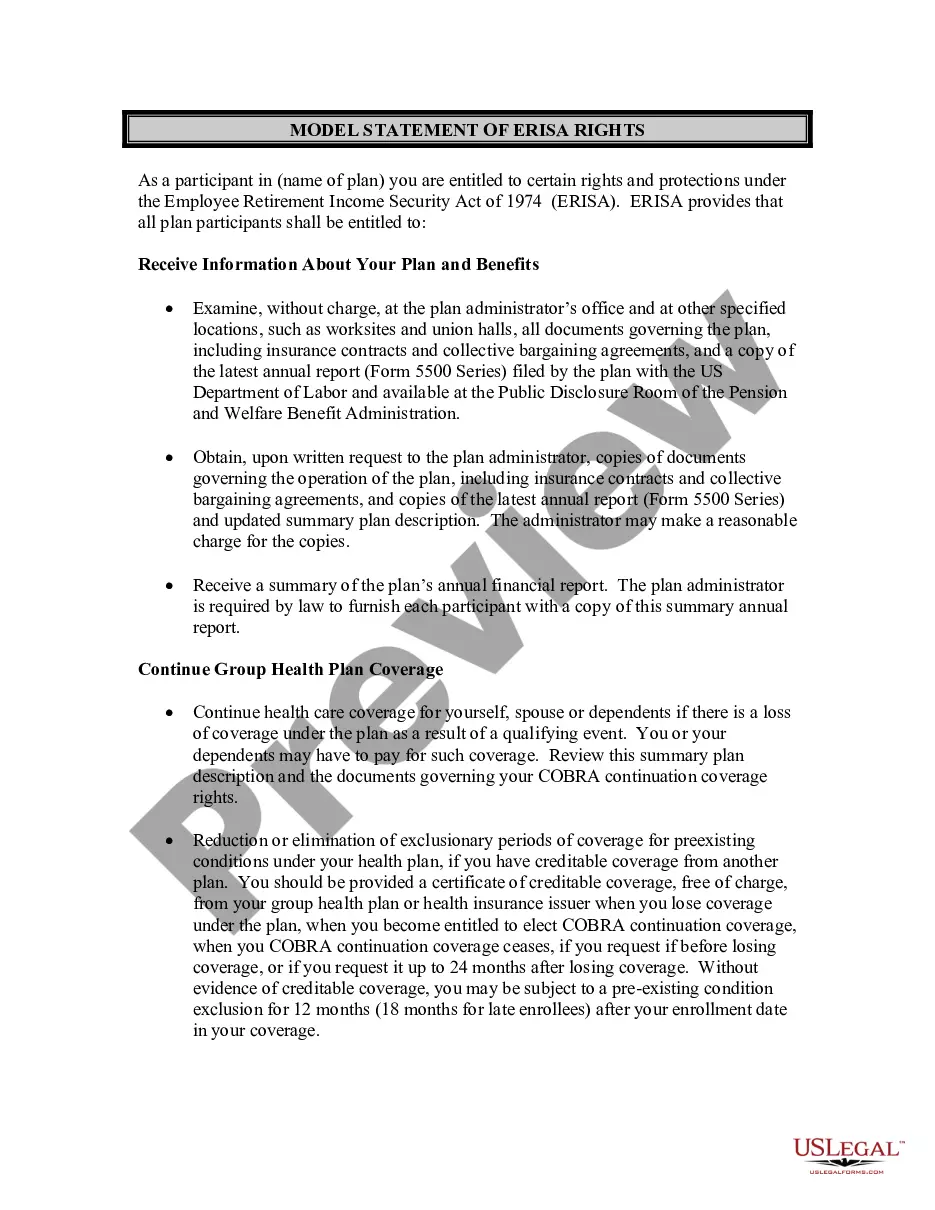
2022 HIPAA allows eligible individuals to enroll in health plan coverage outside of the regular enrollment periods. 2022 These special enrollment rights apply to employees and their dependents, depending on the circumstance.
2022 Birthday Rule: This is a method used to determine when a plan is primary or secondary for a dependent child when covered by both parents' benefit plan. The parent whose birthday (month and day only) falls first in a calendar year is the parent with the primary coverage for the dependent.
If there is a court order that states the parents share joint custody without designating that one parent is responsible for medical expenses, the parent whose birthday falls earliest in the plan year will be primary.
The HIPAA certificate of creditable coverage is no longer a required notice. The certificate was eliminated at the end of 2014 because its primary function was to address pre-existing condition exclusions (PCEs). The ACA has since prohibited all PCEs, which is why the certificate is no longer required.
Prior to 2022, only two states provided Medigap beneficiaries with a birthday rule. Oregon and California were the first. Now, three additional states are implementing birthday rules. These states are Idaho, Illinois, and Nevada.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) Passed in 1985, COBRA is a federal law that allows employees of certain companies to continue their health insurance with the same benefits even after they stop working for their employer.
What is the contract called that is issued to an employer for a Group Medical Insurance plan? (An employer would be a possible applicant and contract policyholder of a single master contract or master policy for group health benefits.)
In general, employers must allow all employees who had at least 1,000 hours of service in the preceding plan year to participate in a simple cafeteria plan. However, employers may exclude from the plan employees who meet one of the following criteria: Are under age 21 before the close of a plan year.
If you get married, you're eligible to get coverage effective the first of the following month, regardless of how late in the month you enroll. If you have a baby, adopt a child, or receive a court order for medical child support, the coverage can be backdated to the date of the birth, adoption, or court order.
The Special Enrollment Period to sign up for Part D (must also enroll in Part A & B) occurs: During the 63 days after employer/union or Veteran's Administration coverage ends, or when the employment ends (whichever is first).