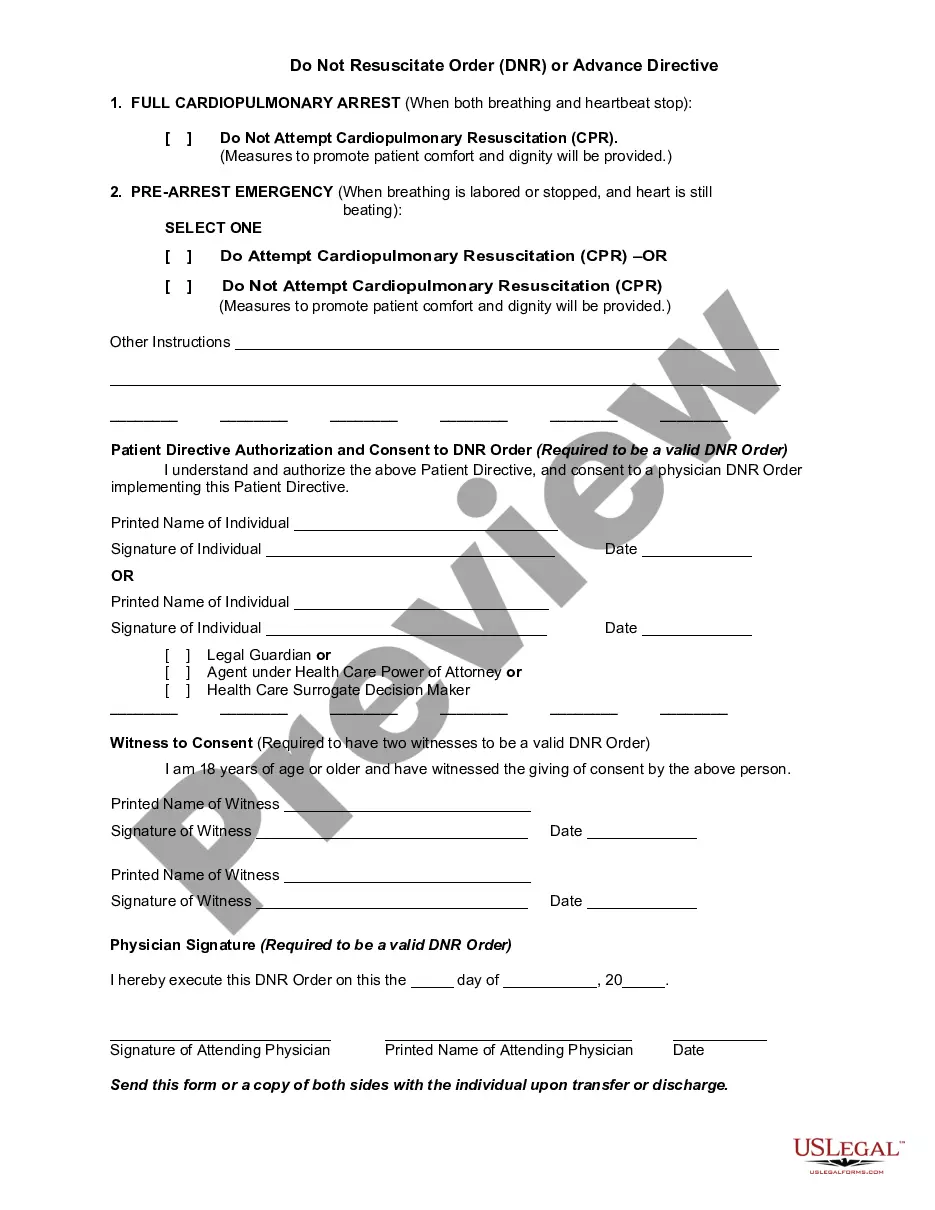
A do not resuscitate (DNR) order is a request not to have cardiopulmonary resuscitation (CPR) if your heart stops or if you stop breathing. Unless given other instructions, hospital staff will try to help all patients whose heart has stopped or who have stopped breathing. A DNR order is put in your medical chart by your doctor. DNR orders are accepted by doctors and hospitals in all states.
This form is a generic example that may be referred to when preparing such a form for your particular state. It is for illustrative purposes only. Local laws should be consulted to determine any specific requirements for such a form in a particular jurisdiction.
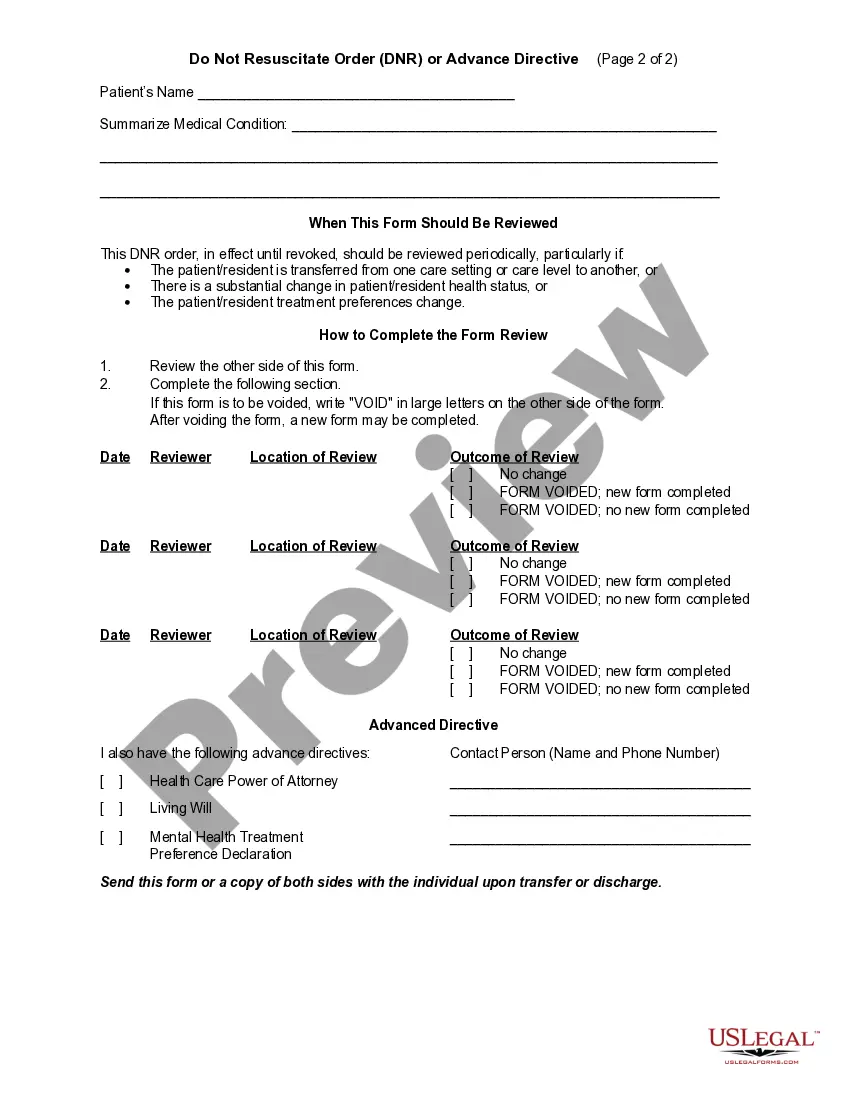
The Virginia Do Not Resuscitate Order (DNR) or Advance Directive is a legal document that allows individuals to express their healthcare preferences when facing life-threatening situations. This detailed description will clarify what a Virginia DNR or Advance Directive entails, its importance, and the different types available in the state. In Virginia, I Do Not Resuscitate Order (DNR) is a medical order allowing patients to refuse certain life-saving interventions. This document is designed for individuals who have a terminal condition, advanced illness, or who wish to have their end-of-life choices respected. It instructs healthcare professionals to not perform cardiopulmonary resuscitation (CPR) or use specific measures to revive the patient in case of cardiac arrest or respiratory failure. A DNR order is valid only during the duration of the current hospital stay or until it is revoked by the patient or their authorized representative. On the other hand, an Advance Directive in Virginia is a comprehensive legal document that addresses more extensive healthcare decisions. Also known as a Living Will, it provides individuals with the opportunity to outline their preferences and instructions regarding medical treatment in various scenarios. An Advance Directive offers guidance to healthcare providers and loved ones for situations where individuals cannot make decisions for themselves due to physical or mental incapacity. It helps ensure that patients' wishes are respected and provides a designated healthcare agent to act on their behalf. Within the realm of Advance Directives, two common types used in Virginia are: 1. Medical Power of Attorney: This type designates a trusted individual as the healthcare agent or proxy to make medical decisions on behalf of the patient when they are unable to do so. The chosen agent should be knowledgeable about the patient's values, beliefs, and desires, and will work closely with healthcare professionals to ensure the patient's directives are followed. 2. Living Will: Unlike a traditional will, a Living Will provides instructions and preferences related to medical treatments, interventions, life-sustaining measures, and end-of-life care choices. It may include desires regarding resuscitation, mechanical ventilation, tube feeding, pain management, and organ donation, among others. Completing a DNR or Advance Directive is a deeply personal and important process as it allows individuals to have a say in their medical care, respecting their own values, beliefs, and priorities. To ensure the legality and validity of these documents, they must be signed by the patient while possessing the necessary mental capacity or by a designated healthcare agent in the presence of two witnesses, preferably not family members. It is crucial to have conversations with family members, loved ones, and healthcare providers to inform them about the existence of a DNR or Advance Directive document and its specific contents. Regular review and revisions are recommended to align the document with the individual's evolving healthcare goals and preferences. In summary, the Virginia Do Not Resuscitate Order (DNR) or Advance Directive is a crucial legal instrument that allows individuals to express their healthcare preferences in life-threatening situations. It encompasses different types, such as Medical Power of Attorney and Living Will, which offer clarity and guidance to healthcare professionals and loved ones. Completing and regularly reviewing these documents ensures that an individual's healthcare wishes are respected and followed when they are unable to advocate for themselves.