South Dakota Hospital Audit Program
Description
How to fill out Hospital Audit Program?
Are you currently in a position where you need documentation for potentially organizational or individual reasons almost every day.
There are numerous legal document templates available online, but finding reliable ones can be challenging.
US Legal Forms offers thousands of form templates, such as the South Dakota Hospital Audit Program, that are designed to meet state and federal requirements.
Select a convenient file format and download your copy.
Access all the document templates you have purchased in the My documents list. You can obtain another copy of the South Dakota Hospital Audit Program at any time, if desired. Click on the required form to download or print the document template. Use US Legal Forms, the most extensive collection of legal forms, to save time and avoid mistakes. The service provides professionally crafted legal document templates that can be utilized for various purposes. Create an account on US Legal Forms and start making your life easier.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- After that, you can download the South Dakota Hospital Audit Program template.
- If you do not have an account and wish to use US Legal Forms, follow these steps.
- Find the form you require and ensure it is for the correct city/state.
- Use the Preview button to review the form.
- Check the details to ensure you have selected the correct document.
- If the form isn’t what you are looking for, utilize the Lookup field to find the one that meets your needs and criteria.
- When you find the appropriate form, click Get now.
- Choose the pricing plan you want, fill in the necessary details to create your account, and complete your order using PayPal or Visa or Mastercard.
Form popularity
FAQ
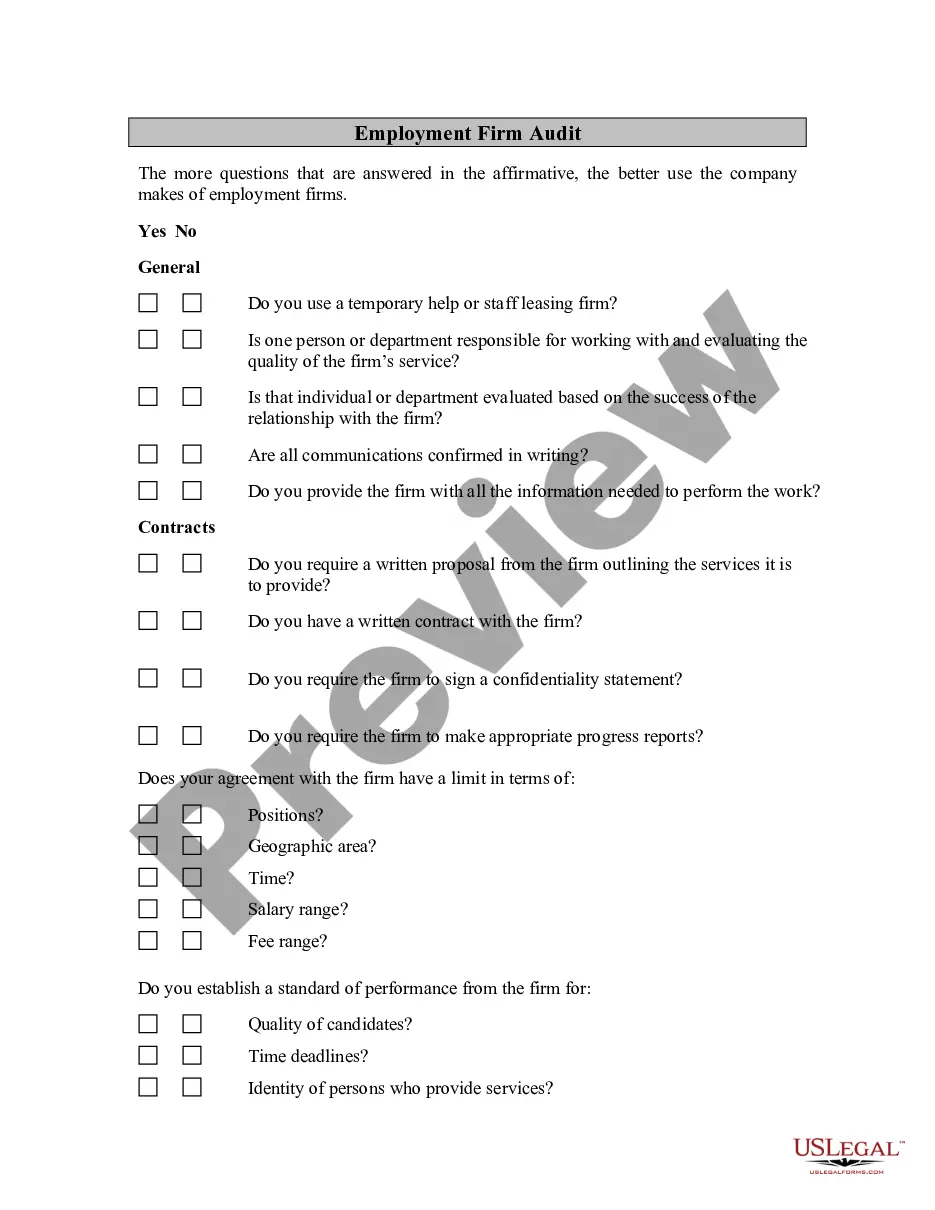
Internal audits are conducted by internal auditors of the hospital's own organisation, such as quality officers or healthcare professionals from another department than the one being audited to guarantee some level of independent judgement.
Audit of Income of HospitalsBills should be verified with the fees/charges structure. Concession and waiver on account of fees and other charges should be verified. Bills should be verified with cash receipt book, counterfoil of receipts and cash book. Verification of arrears of bills should be done.
Auditors Assess Billing Mistakes The problems fall into four categories: insufficient documentation, no documentation, medically unnecessary treatments and overall incorrect coding. There may be plain old administrative mistakes, such as double billings and payments based on incorrect or outdated fee schedules.
One of the primary tasks of the SMRCs is to conduct nationwide medical review as directed by CMS. SMRCs will evaluate medical records and related documents to determine whether Medicare claims were billed in compliance with coverage, coding, payment and billing guidelines.
The Centers for Medicare and Medicaid's audit program is administered by a recovery audit contractor in each of four regions of the United States.
In the case of physician practices, audits are usually performed by Part B carriers. One of the more common methods used by Medicare to determine that an audit is appropriate is through the identification of billing patterns.
Medicare audits are one of several things that can trigger a larger civil or criminal investigation by federal law enforcement. Usually, auditors con- clude that Medicare has made significant over- paymentsand demand that the audited physician return the money.
Outlier payments and higher-than-average use of procedures are likely the most common audit triggers. Some payors compare comparable practices in the same geographic area to one another to study practitioner utilization rates. Being an outlier in this comparison may trigger an audit.
What Triggers a Medicare Audit? A key factor that often triggers an audit is claiming reimbursement for a higher than usual frequency of services over a period of time compared to other health professionals who provide similar services.