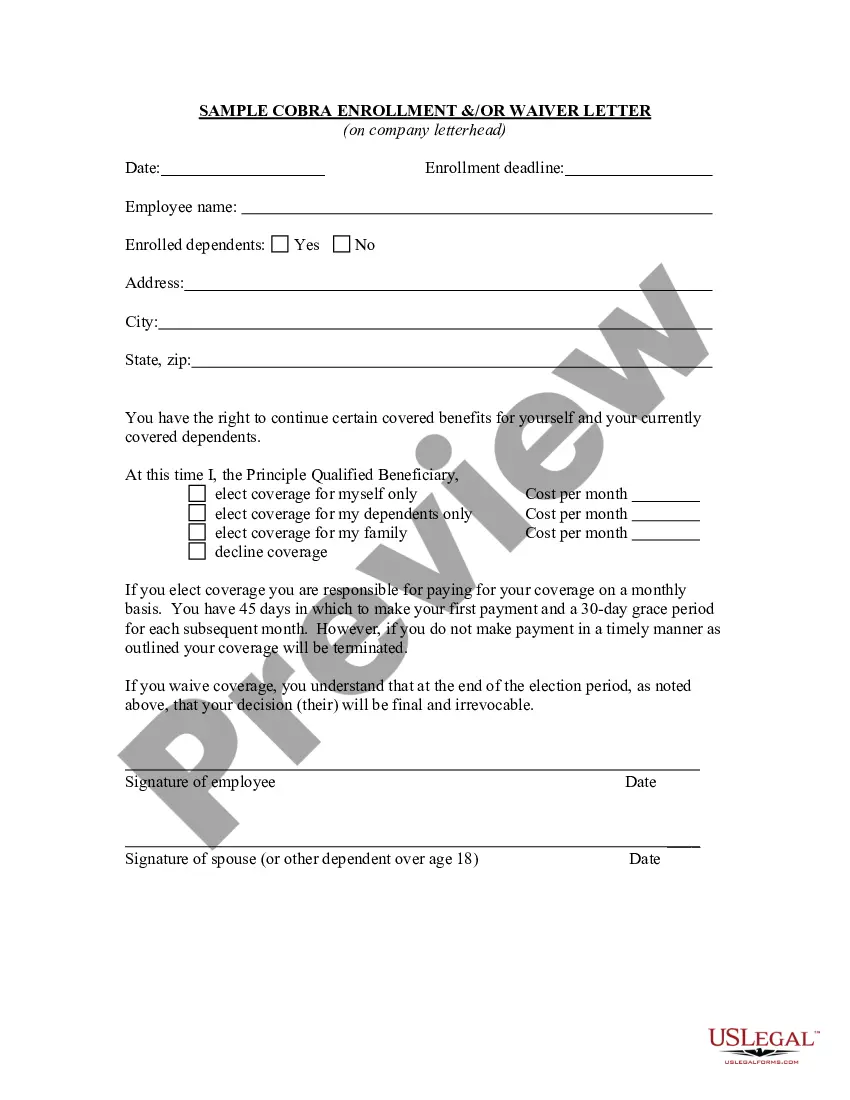
South Carolina COBRA Continuation Waiver Letter
Description
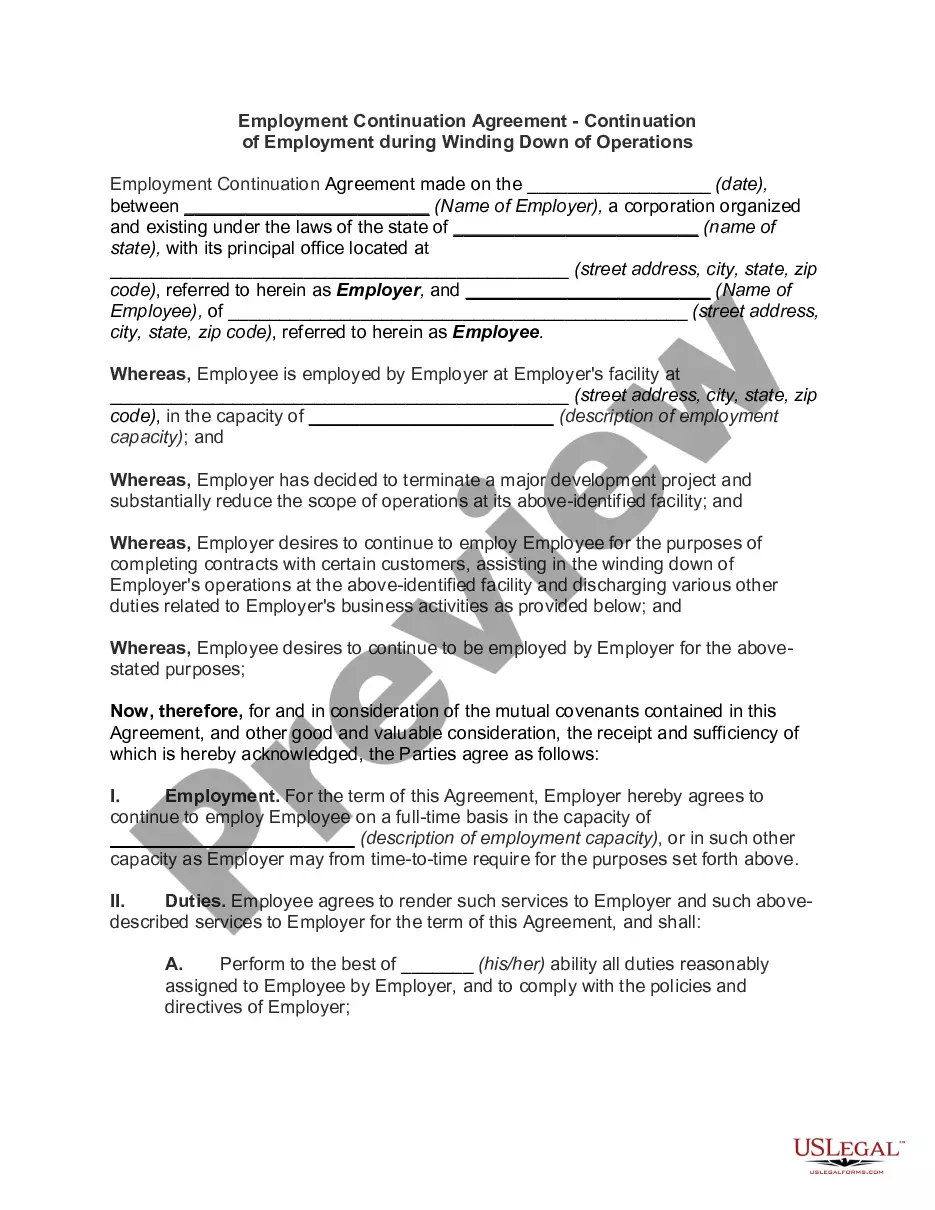
How to fill out COBRA Continuation Waiver Letter?
If you require to aggregate, acquire, or print legal document templates, utilize US Legal Forms, the largest collection of legal forms available online.
Utilize the site’s straightforward and user-friendly search to find the documents you seek. Numerous templates for business and personal purposes are organized by categories and states, or keywords.
Employ US Legal Forms to obtain the South Carolina COBRA Continuation Waiver Letter in just a few clicks.
Every legal document template you purchase is yours indefinitely. You have access to all forms you downloaded in your account. Navigate to the My documents section and select a form to print or download again.
Compete and obtain, and print the South Carolina COBRA Continuation Waiver Letter with US Legal Forms. There are numerous professional and state-specific forms available for your business or personal needs.
- If you are already a US Legal Forms client, Log Into your account and click on the Download option to receive the South Carolina COBRA Continuation Waiver Letter.
- You can also access forms you previously downloaded from the My documents tab of your account.
- If you are using US Legal Forms for the first time, follow the instructions below.
- Step 1. Ensure you have selected the form for the correct region/state.
- Step 2. Utilize the Preview feature to review the form’s content. Be sure to check the particulars.
- Step 3. If you are not satisfied with the form, use the Search section at the top of the screen to find other forms in the legal template.
- Step 4. Once you have found the form you desire, click on the Download now button. Choose the payment plan you prefer and enter your details to register for the account.
- Step 5. Complete the transaction. You can use your credit card or PayPal account to finalize the purchase.
- Step 6. Select the format of the legal form and download it to your device.
- Step 7. Complete, modify, and print or sign the South Carolina COBRA Continuation Waiver Letter.
Form popularity
FAQ
You can cancel your COBRA coverage, but obtaining a refund may not be possible. Typically, COBRA payments are non-refundable unless there was an error in billing or payment processing. To formally cancel your COBRA coverage, you should submit a South Carolina COBRA Continuation Waiver Letter to your plan administrator. This letter will help you document your decision and ensure there are no misunderstandings about your coverage status.
If you want to avoid paying the COBRA cost, go with a short-term plan if you're waiting for approval on another health plan. Choose a Marketplace or independent plan for broader coverage. Choose a high-deductible plan to keep your costs low.
Under COBRA, if you leave your current job, you have the option to continue your health care coverage for up to 18 months. You are required to pay the full premium yourself, even if your employer paid part of your premium while you were employed, and the employer may charge an additional, limited administrative fee.
COBRA Coverage PeriodsYou can cancel the COBRA coverage at any time within 18 months. You're not locked in. You will likely want to drop COBRA once you become eligible for a different health plan, such as if you get another job. If you stop paying premiums, COBRA coverage will end automatically.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Instead, Assistance Eligible Individuals do not have to pay any of the COBRA premium for the period of coverage from April 1, 2021 through September 30, 2021. The premium is reimbursed directly to the employer, plan administrator, or insurance company through a COBRA premium assistance credit.
You May Cancel COBRA At Any Time To cancel your your COBRA coverage you will need to notify your previous employer or the plan administrator in writing. After you stop your COBRA insurance, your former employer should send you a letter affirming termination of that health insurance.
If you waive COBRA coverage during the election period, you must be permitted later to revoke your waiver of coverage and to elect continuation coverage as long as you do so during the election period. Then, the plan need only provide continuation coverage beginning on the date you revoke the waiver.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.