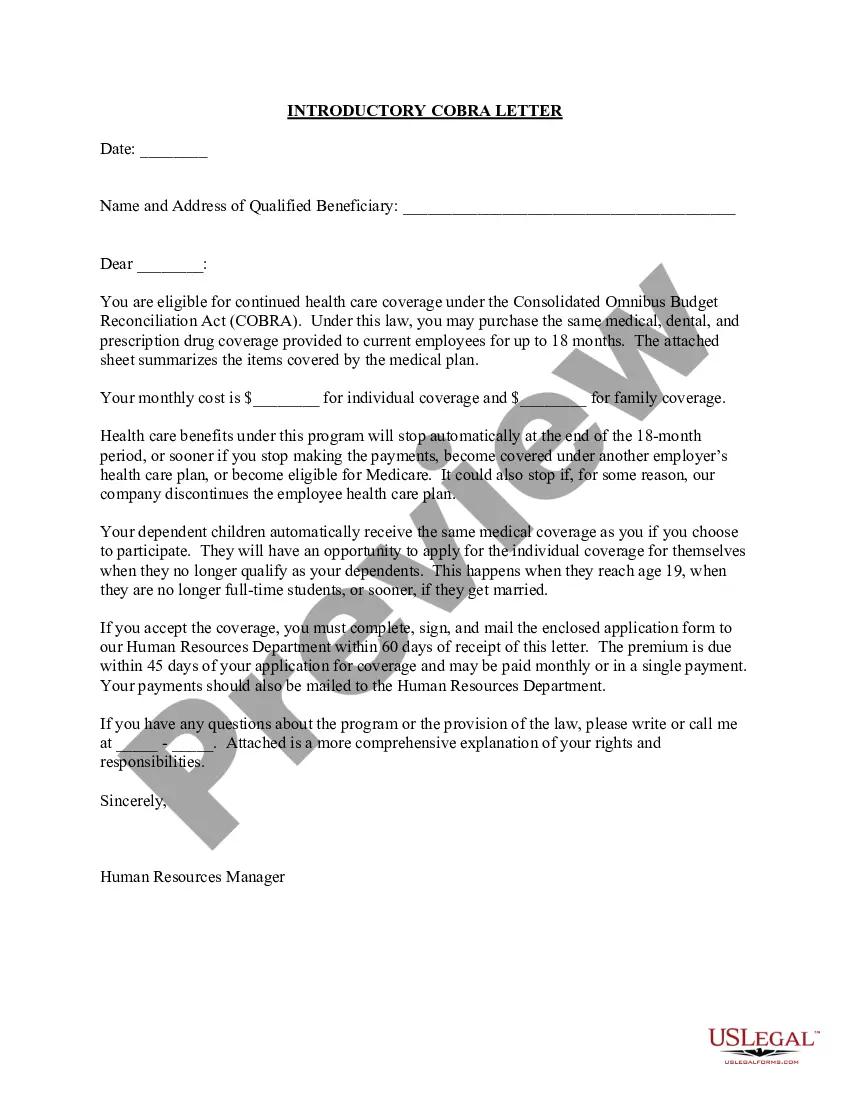
South Carolina Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
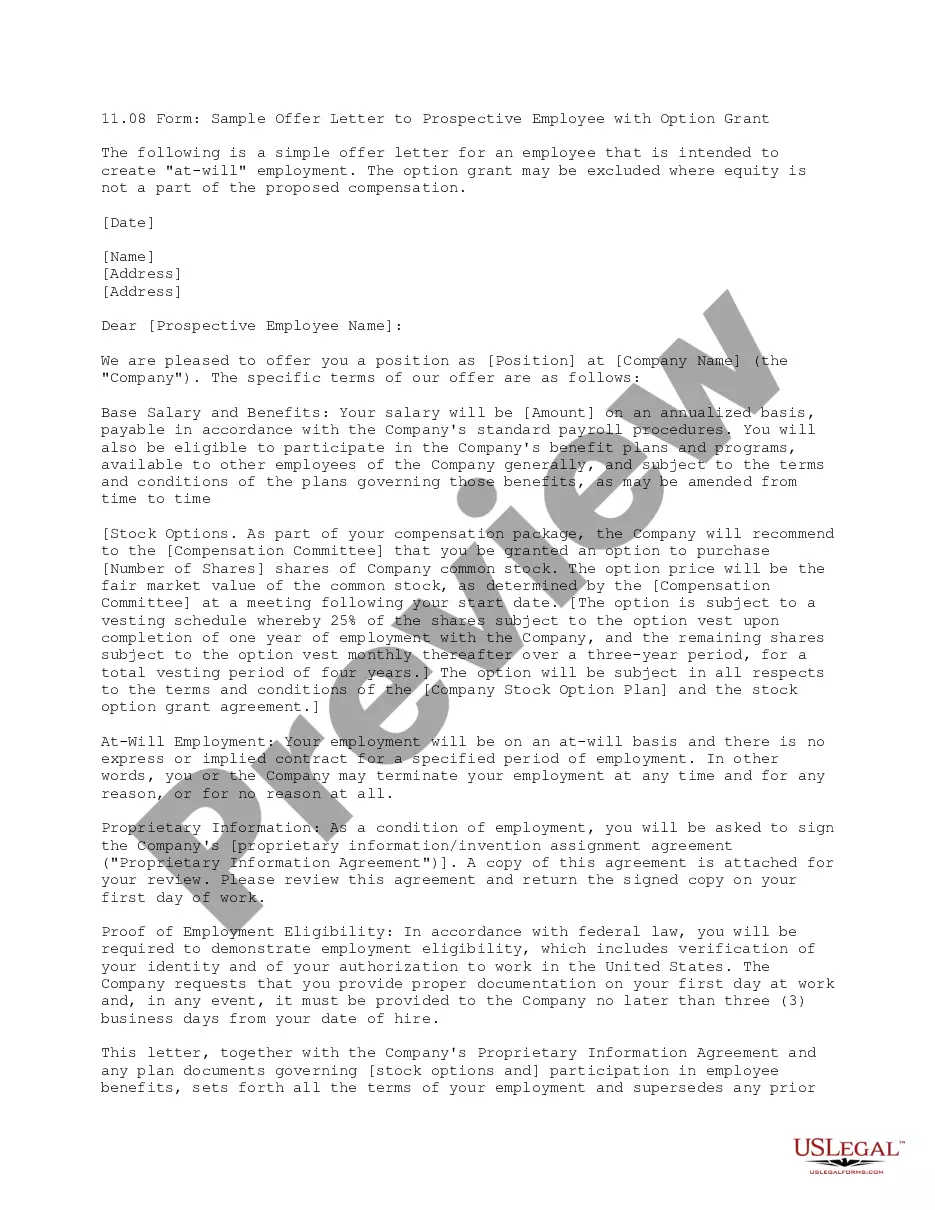
You can spend hours online searching for the legal document template that meets the federal and state requirements you need.
US Legal Forms provides a vast number of legal forms that are vetted by experts.
You can easily download or print the South Carolina Introductory COBRA Letter from my services.
If available, utilize the Review button to browse through the document template as well.
- If you have a US Legal Forms account, you can Log In and click the Download button.
- Then, you can fill out, modify, print, or sign the South Carolina Introductory COBRA Letter.
- Every legal document template you acquire is yours permanently.
- To get another copy of any purchased form, go to the My documents tab and click the corresponding button.
- If you're using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure you have selected the right document template for your region/area of interest.
- Check the form description to verify you have chosen the correct form.
Form popularity
FAQ
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
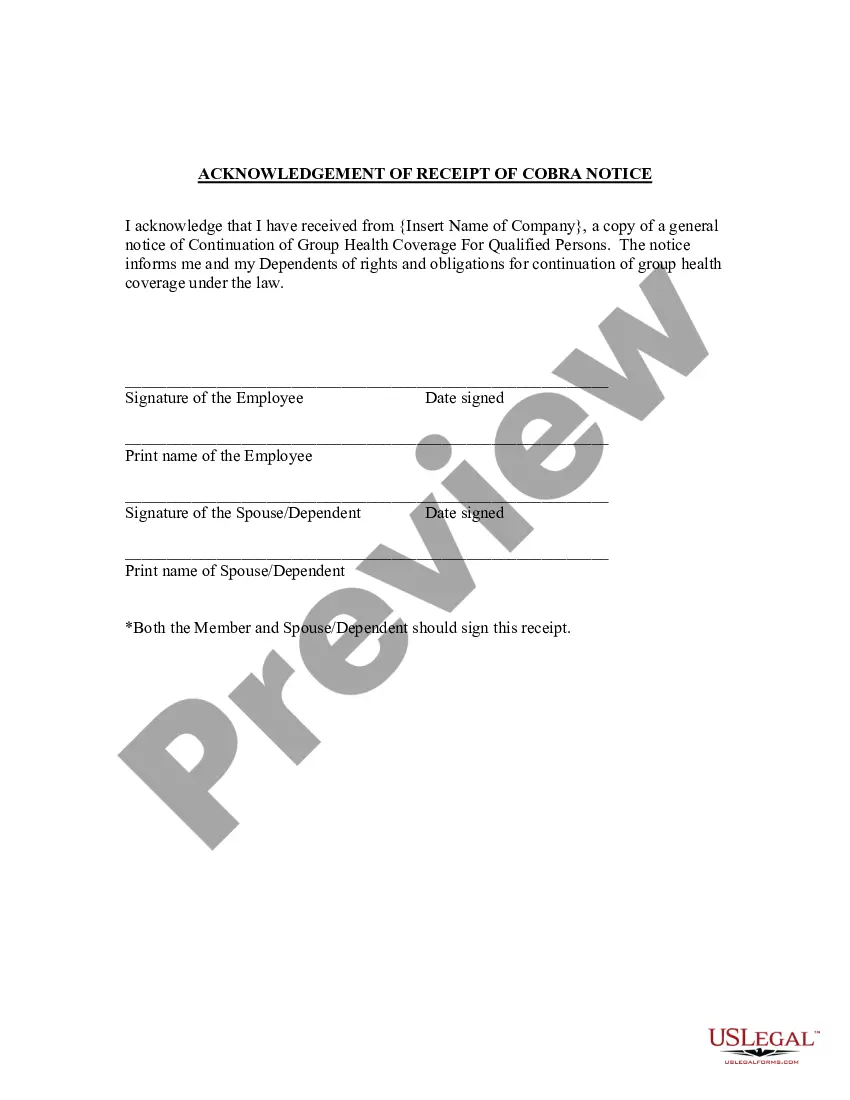
The Consolidated Omnibus Budget Reconciliation Act (COBRA) permits employees and their dependents to extend health coverage under an employer's group health plan when coverage would otherwise be lost due to termination of employment or other qualifying events. Under COBRA, employees must receive specific notices
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
Under COBRA, if you leave your current job, you have the option to continue your health care coverage for up to 18 months. You are required to pay the full premium yourself, even if your employer paid part of your premium while you were employed, and the employer may charge an additional, limited administrative fee.
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive. You are now responsible for the entire insurance premium, whereas your previous employer subsidized a portion of that as a work benefit.
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,