Oklahoma Acknowledgment of Receipt of COBRA Notice
Description
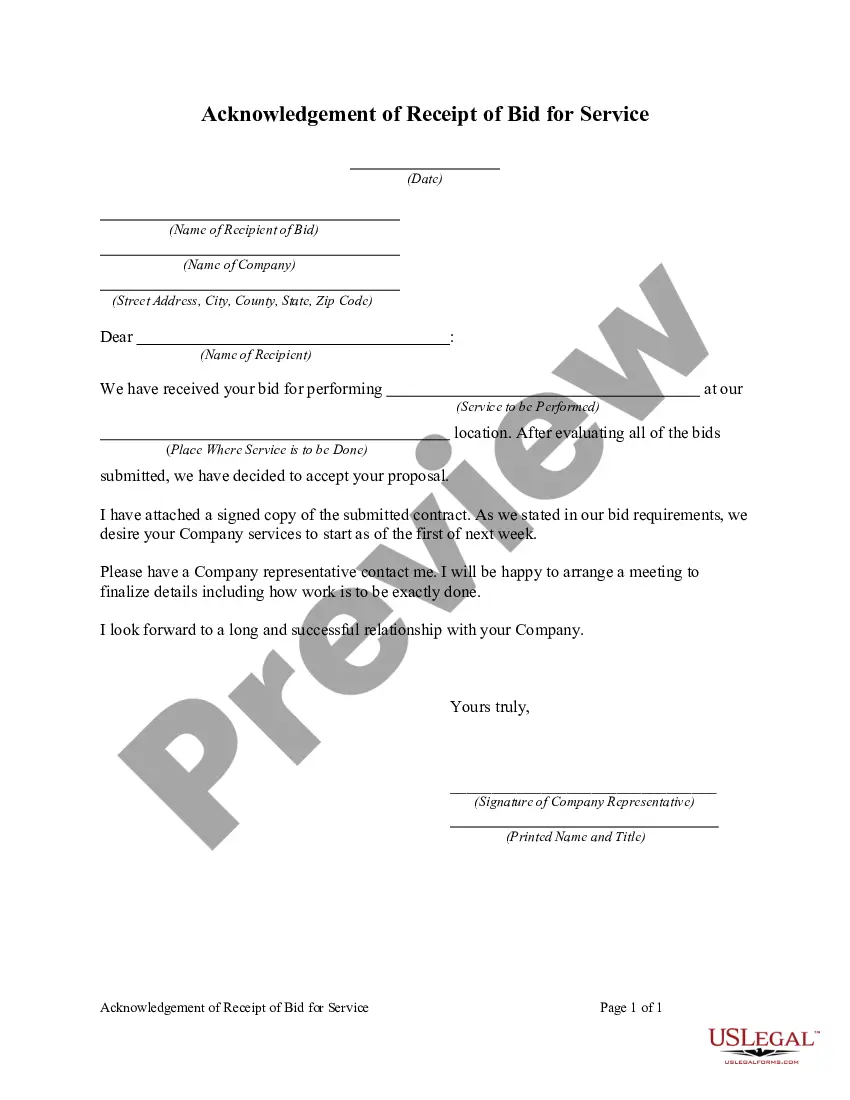
How to fill out Acknowledgment Of Receipt Of COBRA Notice?
If you wish to finalize, obtain, or print legal document templates, utilize US Legal Forms, the most extensive collection of legal forms, available online.
Employ the site’s user-friendly and convenient search to find the documents you require.
A range of templates for business and personal purposes are organized by categories and states, or keywords.
Step 3. If you are not satisfied with the form, use the Search bar at the top of the screen to find other versions of the legal form template.
Step 4. Once you have found the form you need, click the Get Now button. Choose your pricing plan and enter your details to register for an account.
- Utilize US Legal Forms to find the Oklahoma Acknowledgment of Receipt of COBRA Notice with just a few clicks.
- If you are currently a US Legal Forms member, Log In to your account and click on the Download button to obtain the Oklahoma Acknowledgment of Receipt of COBRA Notice.
- You may also access forms you previously saved in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the instructions below.
- Step 1. Ensure you have selected the form for your correct city/state.
- Step 2. Use the Review feature to inspect the form’s content. Remember to read the description.
Form popularity
FAQ
You may be able to keep your job-based health plan through COBRA continuation coverage. COBRA is a federal law that may let you pay to stay on your employee health insurance for a limited time after your job ends (usually 18 months). You pay the full premium yourself, plus a small administrative fee.
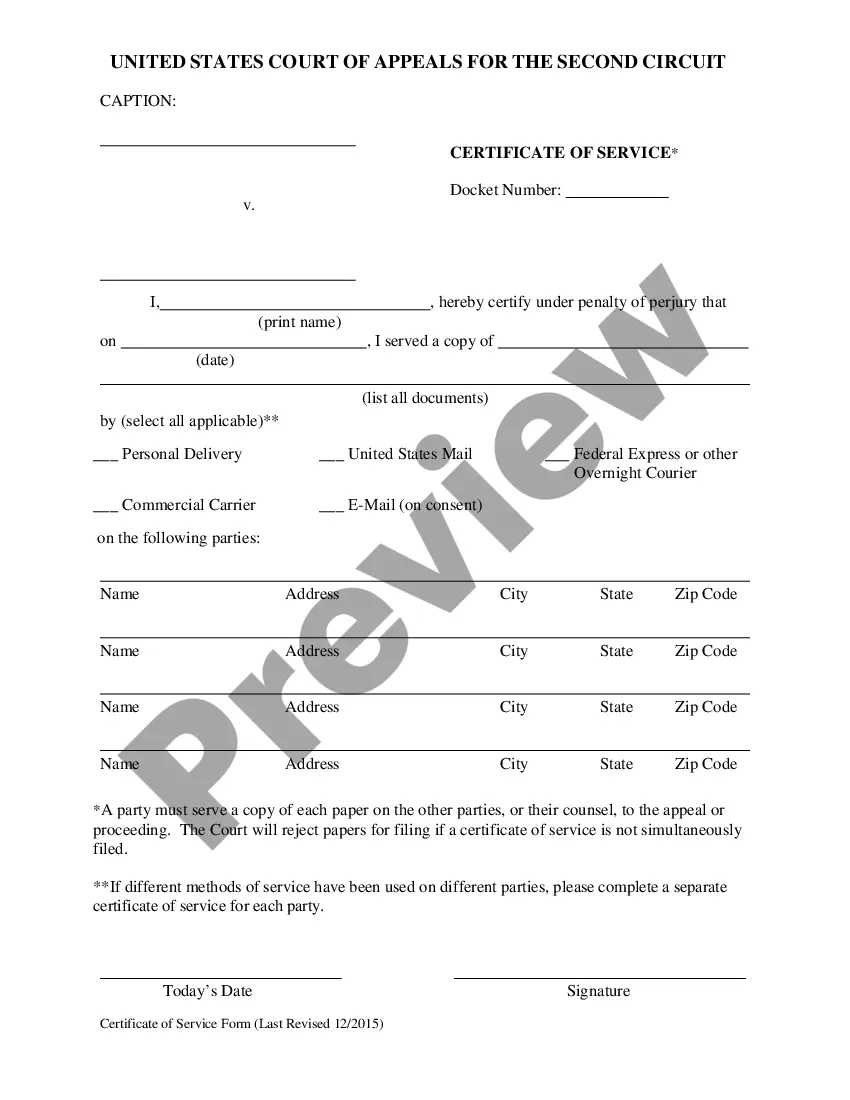
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
Failure to pay premiums. When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Otherwise, when the qualifying event is the end of employment or reduction of the employee's hours of employment, COBRA continuation coverage generally lasts for only up to a total of 18 months. There are two ways in which this 18-month period of COBRA continuation coverage can be extended.
Oklahoma requires limited continuation of healthcare plan coverage for employees whose employer is not covered by the federal Consolidated Omnibus Budget Reconciliation Act (COBRA) (OK Stat. Tit. 36 Sec. 4509).
COBRA is a federal law that lets you keep yourself and your family covered by your employee health plan. Coverage is only available for a limited time (often 18 months) after you leave your job or lose coverage through your employer. You pay the full monthly premium, including any amount that your employer had paid.
The COBRA Rights Notification Letter Template contains a model form of the letter that all employees must receive either from their employer or from the benefit plan administrator of their benefit plans.
If you need further information about COBRA, ACA, HIPAA, or ERISA, visit the Employee Benefits Security Administration's (EBSA) Website at dol.gov/ebsa/complianceassistance.html. Or you may contact EBSA electronically at askebsa.dol.gov or call toll free 1-866-444-3272.
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive.