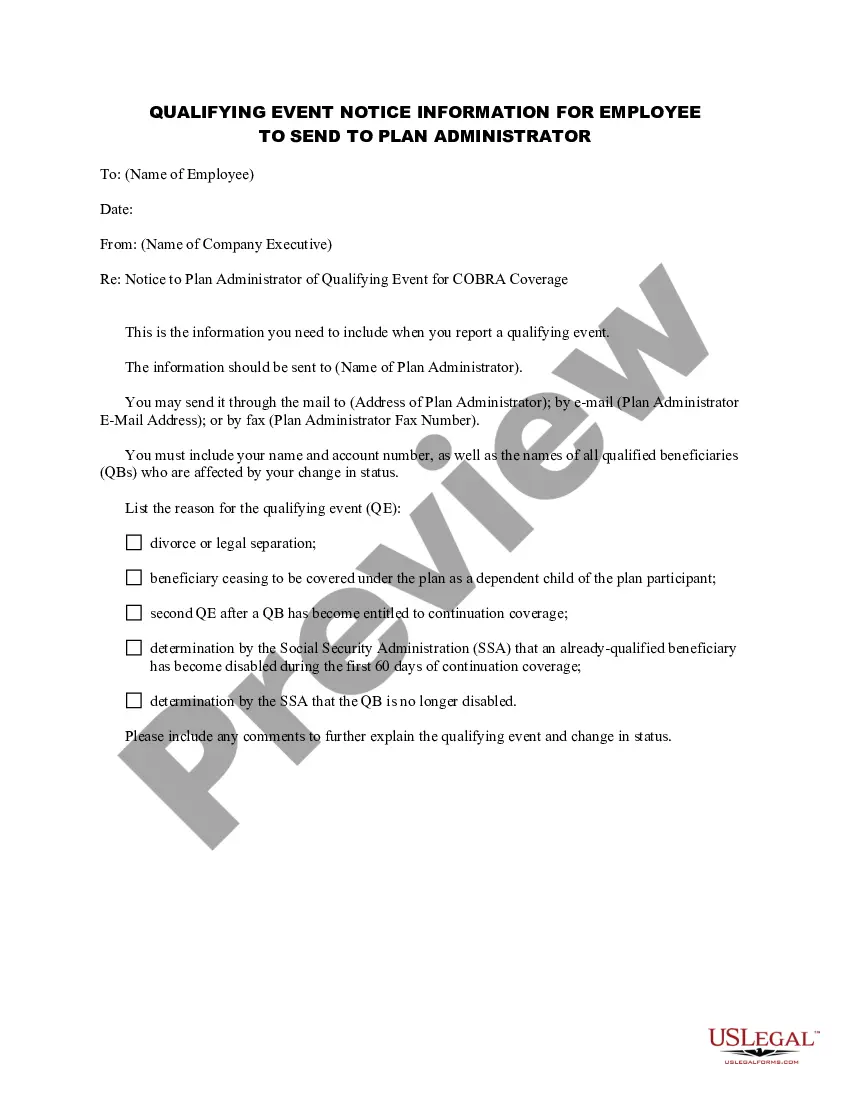
Ohio Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
If you require thorough, acquire, or generate legal document templates, utilize US Legal Forms, the most significant collection of legal forms available online.
Take advantage of the site's straightforward and user-friendly search to find the documents you need.
Many templates for business and personal purposes are organized by categories and states, or keywords.
Step 5. Process the payment. You may use your credit card or PayPal account to complete the transaction.
Step 6. Select the format of the legal form and download it to your device. Step 7. Complete, modify, and print or sign the Ohio Notice of Qualifying Event from Employer to Plan Administrator. Each legal document template you purchase is yours indefinitely. You have access to every form you downloaded in your account. Check the My documents section and choose a form to print or download again. Accomplish and download, and print the Ohio Notice of Qualifying Event from Employer to Plan Administrator with US Legal Forms. There are numerous professional and state-specific forms available for your business or personal needs.
- Employ US Legal Forms to access the Ohio Notice of Qualifying Event from Employer to Plan Administrator in just a few clicks.
- If you are already a US Legal Forms user, Log In to your account and click on the Obtain button to locate the Ohio Notice of Qualifying Event from Employer to Plan Administrator.
- You can also retrieve forms you previously submitted electronically in the My documents tab of your account.
- If you are using US Legal Forms for the first time, follow the instructions below.
- Step 1. Ensure you have selected the form for the correct region/country.
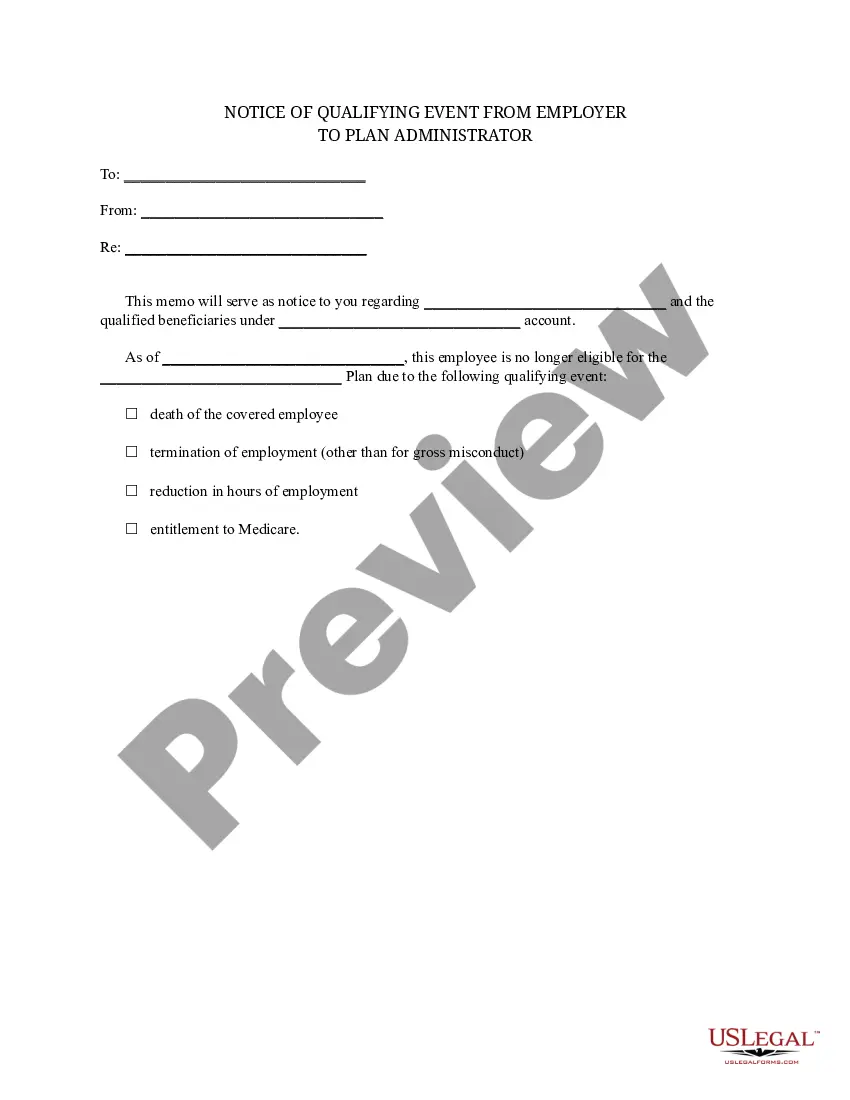
- Step 2. Utilize the Preview option to review the form's content. Be sure to read the description.
- Step 3. If you are unsatisfied with the form, use the Search field at the top of the screen to find additional versions of the legal form template.
- Step 4. Once you have found the form you desire, select the Purchase now button. Choose your preferred pricing plan and enter your credentials to register for an account.
Form popularity
FAQ
COBRA coverage in Ohio typically lasts for 18 months for most qualified individuals, but it can extend up to 36 months for certain circumstances. When a qualifying event occurs, the employer should provide an Ohio Notice of Qualifying Event from Employer to Plan Administrator to help you understand your rights. Knowing the duration of your COBRA coverage is essential in planning your healthcare needs, and uslegalforms can assist you in navigating your options.
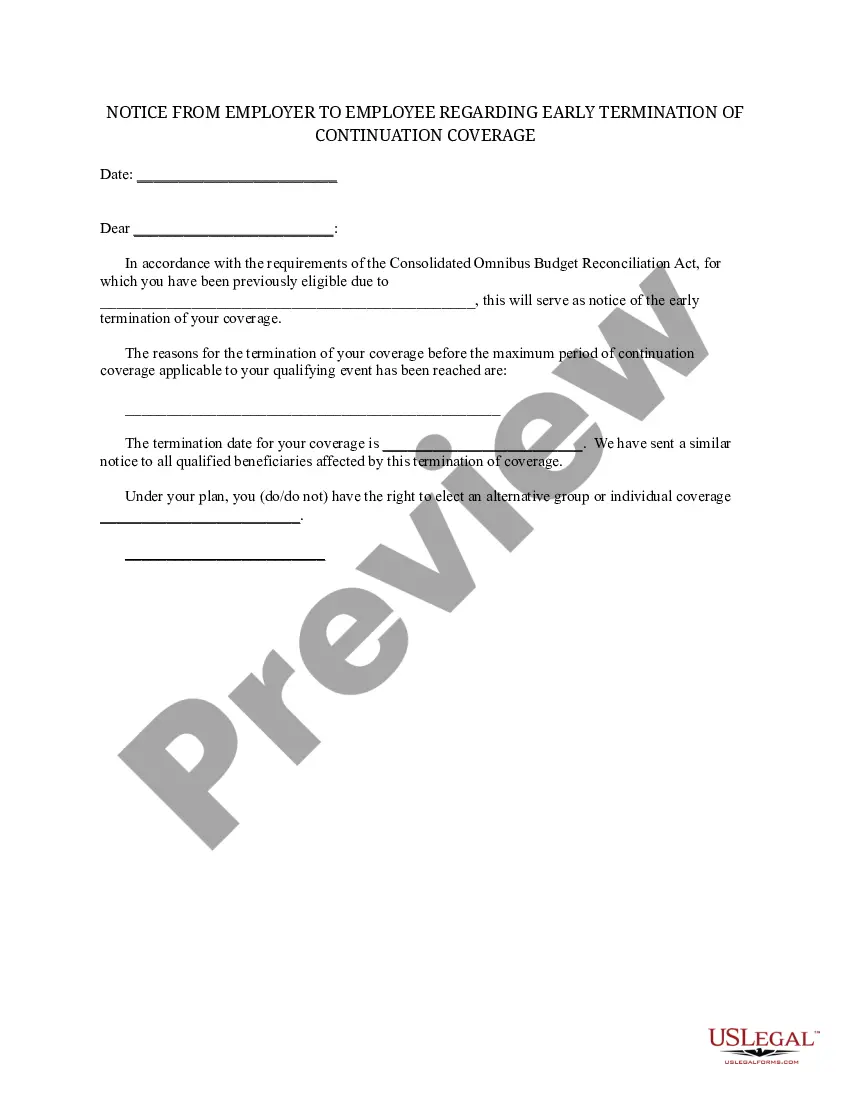
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
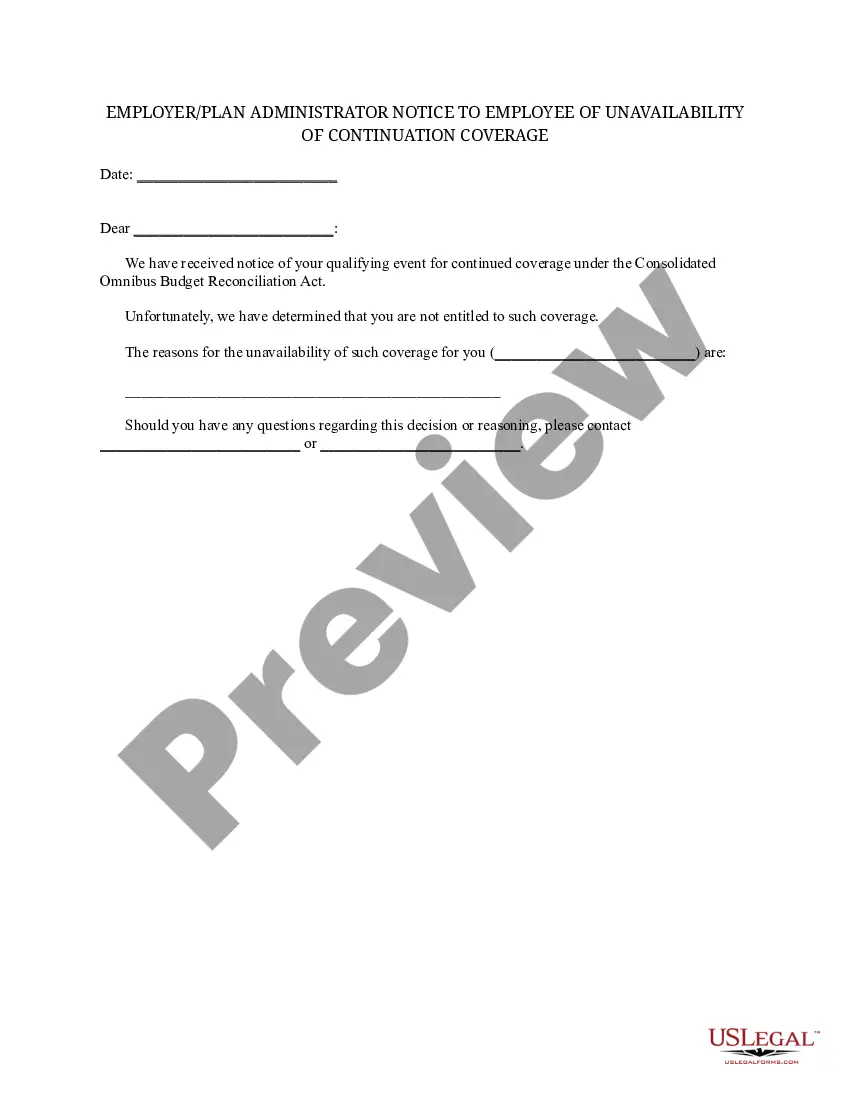
Failure to pay premiums. When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
(An employer MUST have 20 employees for a terminated employee to be eligible for COBRA.)