New Hampshire Summary of Rights and Obligations under COBRA
Description
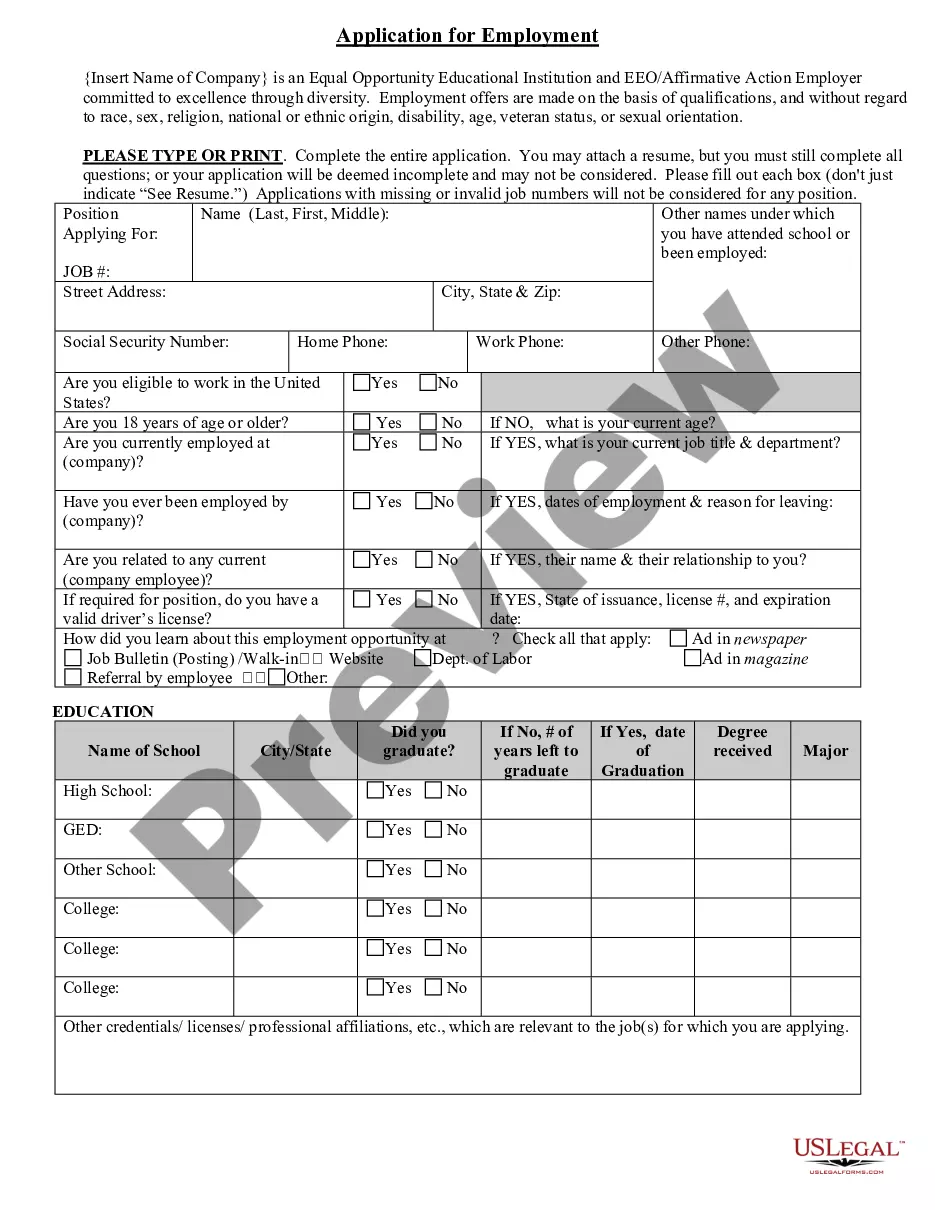
How to fill out Summary Of Rights And Obligations Under COBRA?
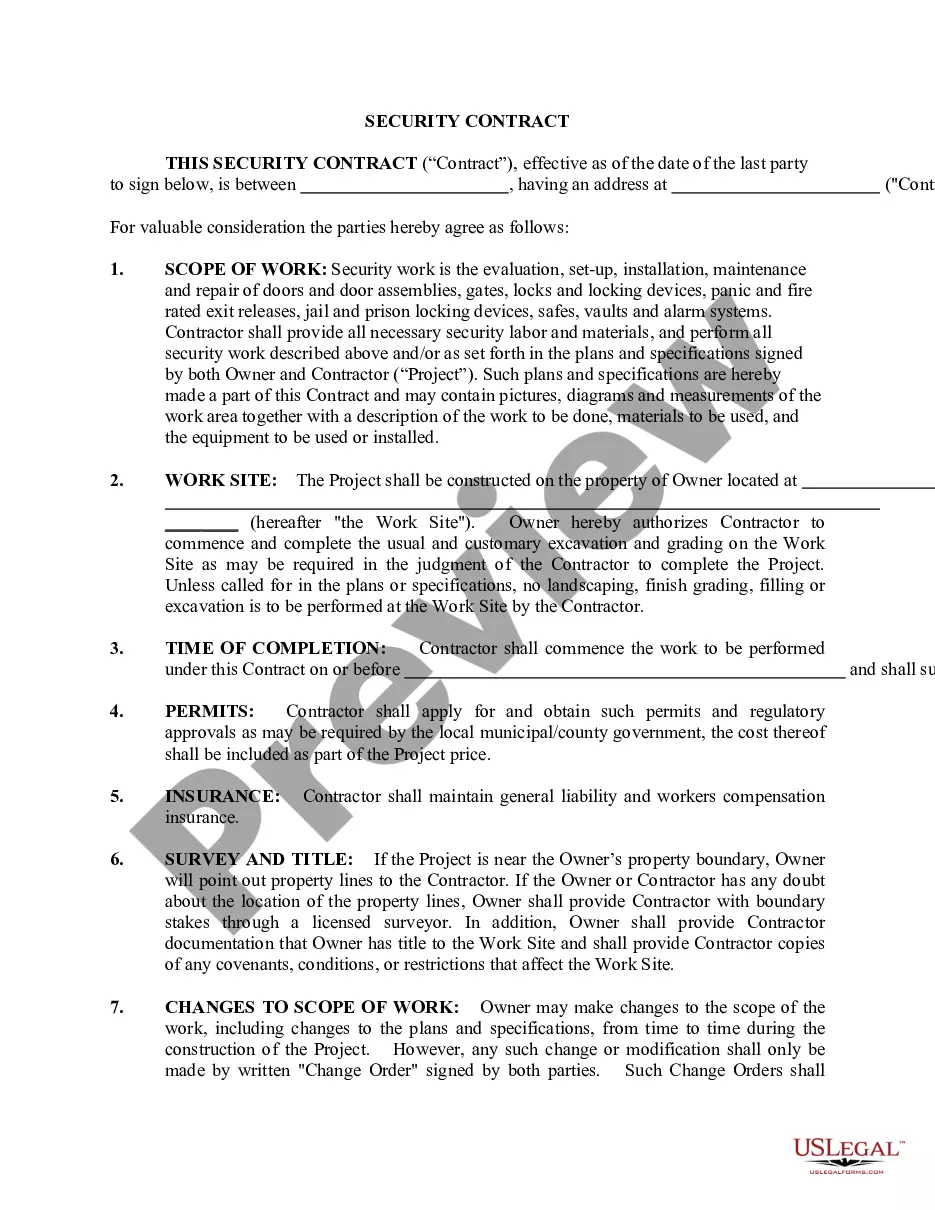
You might spend numerous hours online trying to locate the legal document template that meets both federal and state requirements you require.
US Legal Forms provides thousands of legal templates that can be reviewed by experts.
You can actually obtain or generate the New Hampshire Summary of Rights and Obligations under COBRA from the service.
If available, make use of the Preview button to review the document template at the same time.
- If you have a US Legal Forms account, you can Log In and click on the Download button.
- Afterward, you can fill out, modify, generate, or sign the New Hampshire Summary of Rights and Obligations under COBRA.
- Every legal document template you purchase is yours permanently.
- To receive another copy of the purchased form, go to the My documents tab and click on the appropriate button.
- If you are using the US Legal Forms site for the first time, follow the simple instructions provided below.
- First, ensure you have selected the correct document template for the location/city of your choice.
- Check the form description to confirm you have chosen the right template.
Form popularity
FAQ
In New Hampshire, COBRA coverage can last for up to 18 months for employees who have lost their job or experienced a reduction in hours. This period may extend under certain conditions, such as when a qualifying event affects other family members. It's important to understand your New Hampshire Summary of Rights and Obligations under COBRA, as it outlines your options for continuing health insurance coverage. If you need assistance navigating your rights, uSLegalForms can provide the necessary resources.
Your employer may have just begun offering a health insurance plan. Your employer may have recently hired several new employees, and the increase in the number of employees may force your employer to follow these regulations for the first time.
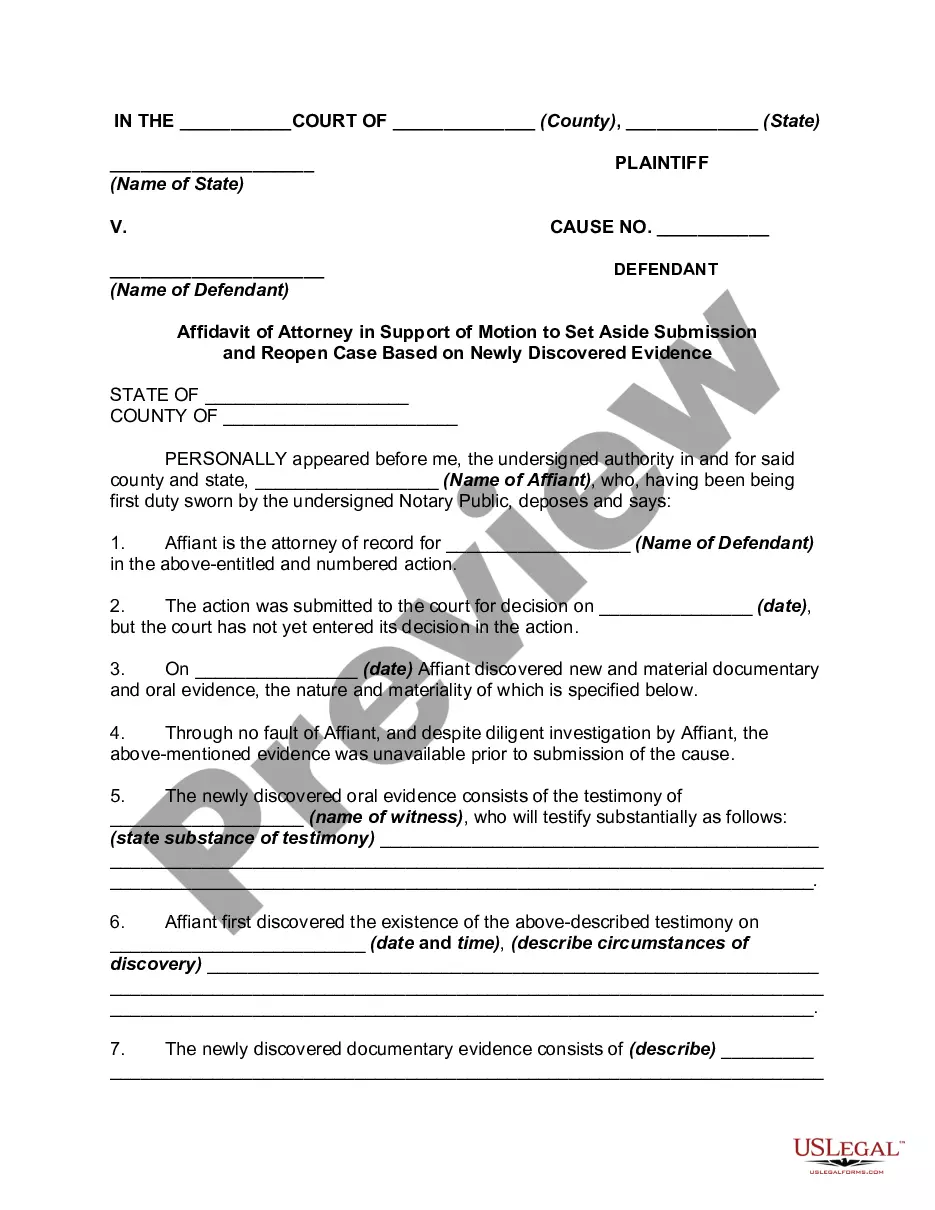
The COBRA Rights Notification Letter Template contains a model form of the letter that all employees must receive either from their employer or from the benefit plan administrator of their benefit plans.
Consumers may also extend COBRA coverage longer than the initial 18-month period with a second qualifying event (e.g., divorce or death), up to an additional 18 months, for a total of 36 months.
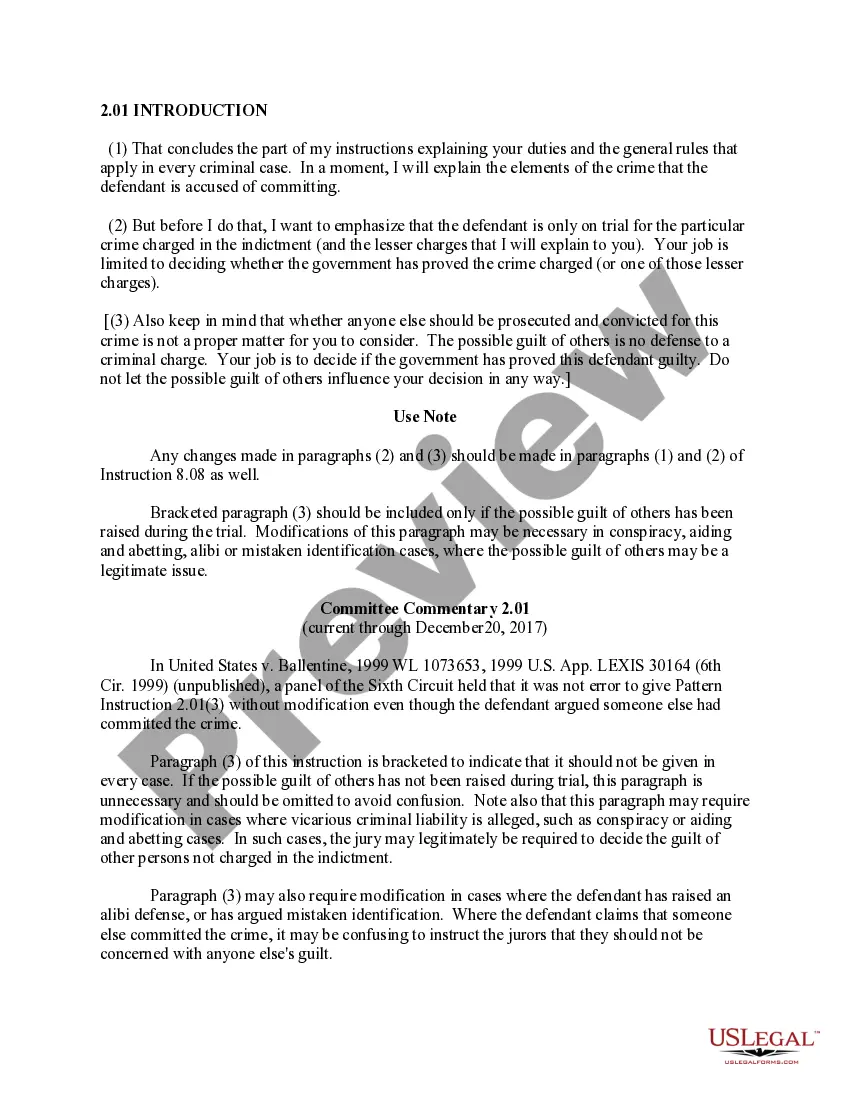
Federal COBRA & New Hampshire Continuation of Coverage Consolidated Omnibus Budget Reconciliation Act Continuation Coverage (COBRA) is a Federal law that gives employees and their covered dependents, who lose health benefits, the right to continue their coverage, in most cases, a maximum of 18 months.
The American Rescue Plan Act and COBRA AssistanceARPA creates a new 100 percent subsidy for COBRA coverage premiums from April 1, 2021, through September 30, 2021. Additionally, ARPA opens up the ability to enroll in COBRA coverage even if a person declined coverage earlier or if their enrollment window closed.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
How Long Does COBRA Last After You Quit? You may remain on your former employer's COBRA insurance plan for up to 18 months. Depending on your circumstances you or your qualified dependents may be eligible for up to 36 months of continuing coverage.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,