Mississippi Anchor Provider Agreement
Description
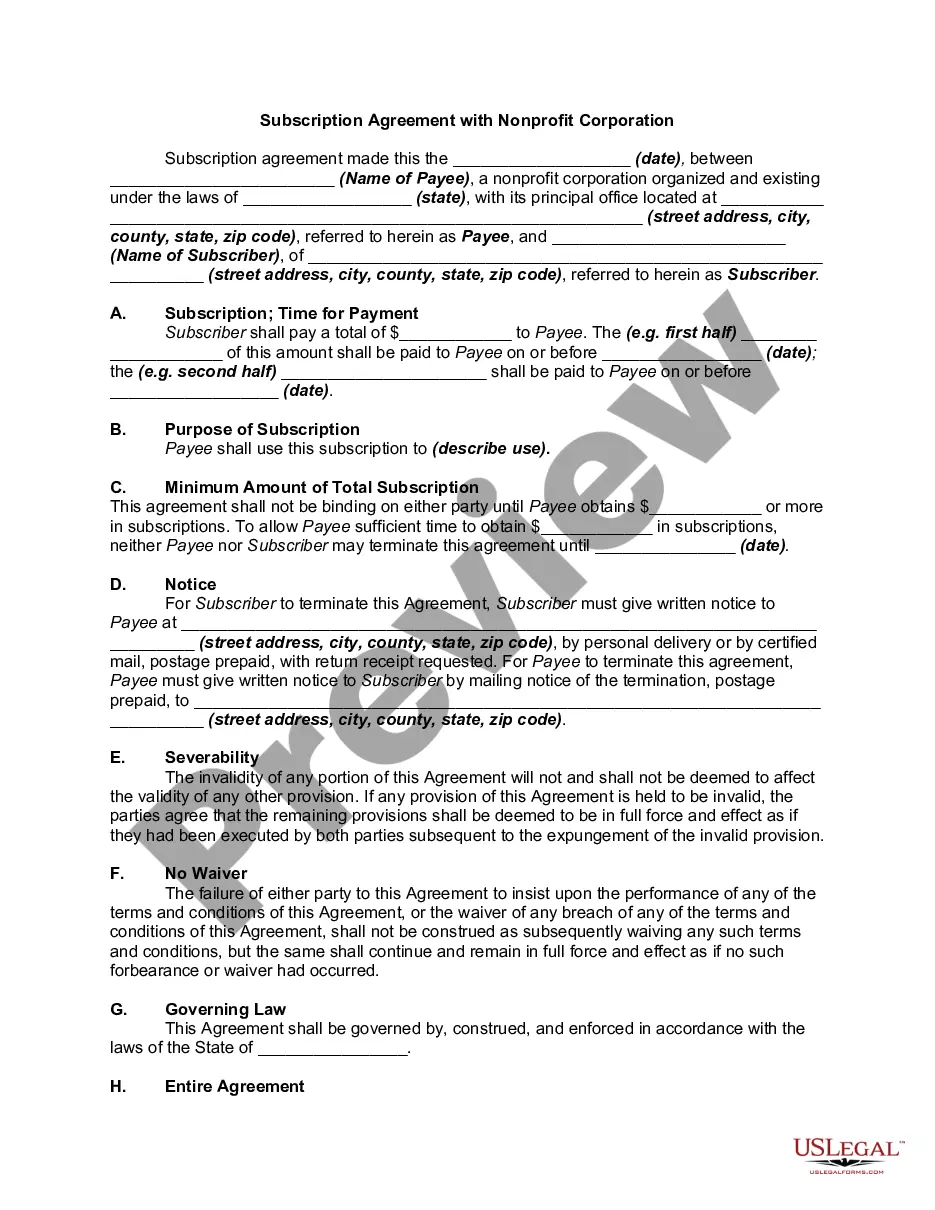
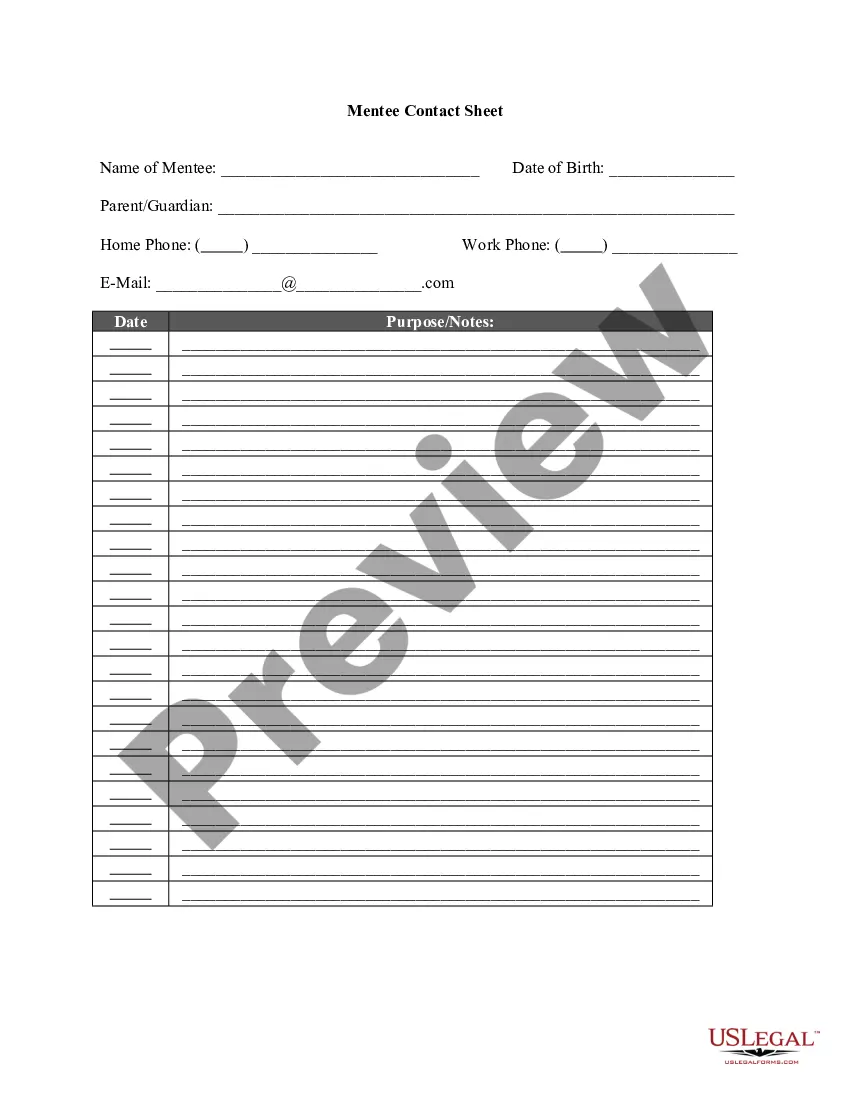
How to fill out Anchor Provider Agreement?
Choosing the right authorized record design can be quite a battle. Of course, there are tons of web templates available on the net, but how would you find the authorized develop you want? Take advantage of the US Legal Forms web site. The service provides a large number of web templates, like the Mississippi Anchor Provider Agreement, which can be used for organization and personal requires. All the varieties are checked out by specialists and fulfill federal and state demands.
If you are currently listed, log in to the bank account and then click the Down load switch to find the Mississippi Anchor Provider Agreement. Make use of your bank account to look through the authorized varieties you may have acquired in the past. Proceed to the My Forms tab of your own bank account and obtain another copy in the record you want.
If you are a fresh consumer of US Legal Forms, allow me to share basic recommendations so that you can stick to:
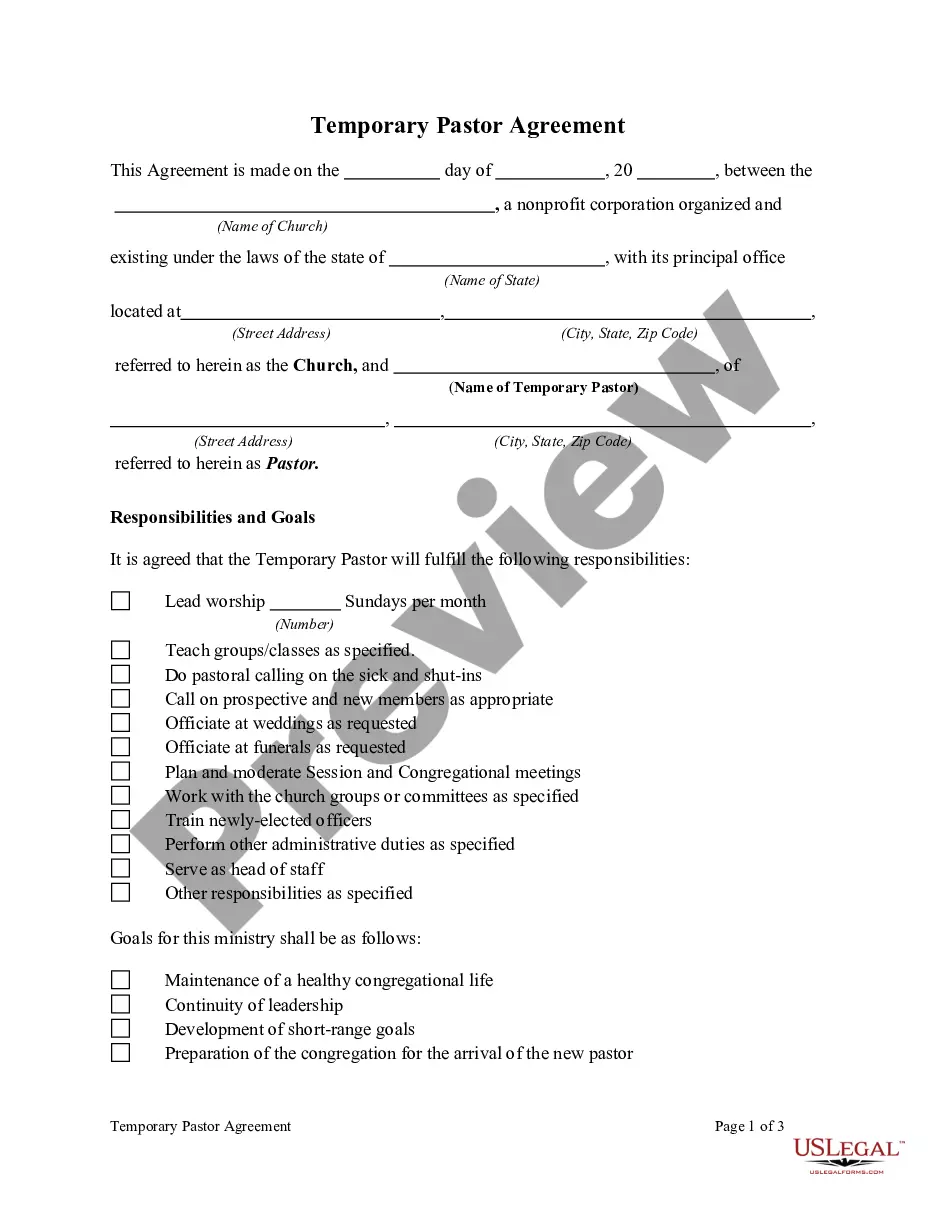
- First, be sure you have chosen the appropriate develop to your town/region. You can look over the form using the Review switch and study the form outline to ensure this is basically the best for you.
- In case the develop will not fulfill your preferences, make use of the Seach area to find the proper develop.
- When you are sure that the form is proper, click on the Get now switch to find the develop.
- Choose the rates program you want and enter in the necessary info. Design your bank account and buy the order with your PayPal bank account or bank card.
- Pick the file formatting and obtain the authorized record design to the device.
- Complete, edit and print out and indication the attained Mississippi Anchor Provider Agreement.
US Legal Forms is the biggest catalogue of authorized varieties where you can discover numerous record web templates. Take advantage of the service to obtain appropriately-made papers that stick to status demands.
Form popularity
FAQ
Contact. For providers or beneficiaries who need to contact the Mississippi Division of Medicaid, please use the below contact information. If you speak another language, assistance services, free of charge, are available to you. Call 1-800-421-2408 (Deaf and Hard of Hearing VP: 1-228-206-6062).
Income Limits for Medicaid and CHIP Programs Family Size12Monthly Income$1,799$2,432
By Email: Email the change or update to: Medicaid.application@medicaid.ms.gov. By Fax: Fax the information to the Bureau of Eligibility at: (601) 576-4164. By Phone: Call the regional office that handles your case at the number, or the Bureau of Eligibility toll-free at (800) 421-2408.
A: No. Because each state has its own Medicaid eligibility requirements, you can't just transfer coverage from one state to another, nor can you use your Medicaid coverage when you're temporarily visiting another state, unless you need emergency health care.
REGULAR REDETERMINATIONS OR RENEWALS ? MAGI & ABD Federal regulations require that the eligibility of every Medicaid and CHIP recipient be reviewed at least every 12 months. Mississippi state law also requires annual reviews.
Filing Limit Claims should be sent to Molina Healthcare within 90 days from the date of service. For resubmission or secondary claims, Molina Healthcare must receive the claim within 180 days from the date of service.
Mississippi Medicaid includes multiple health benefits programs administered by DOM: fee-for-service Medicaid, MississippiCAN and CHIP. The federal medical assistance percentage (FMAP) is used to calculate federal matching funds for medical service expenditures.
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided.