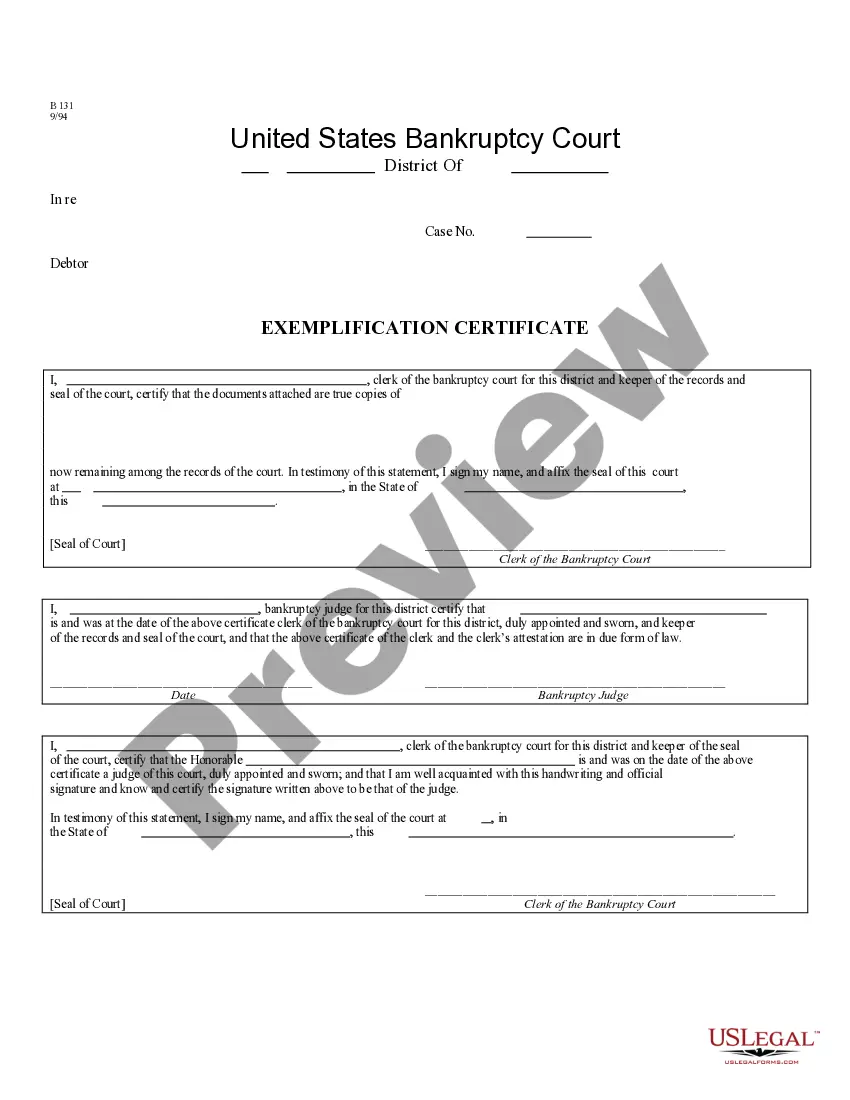
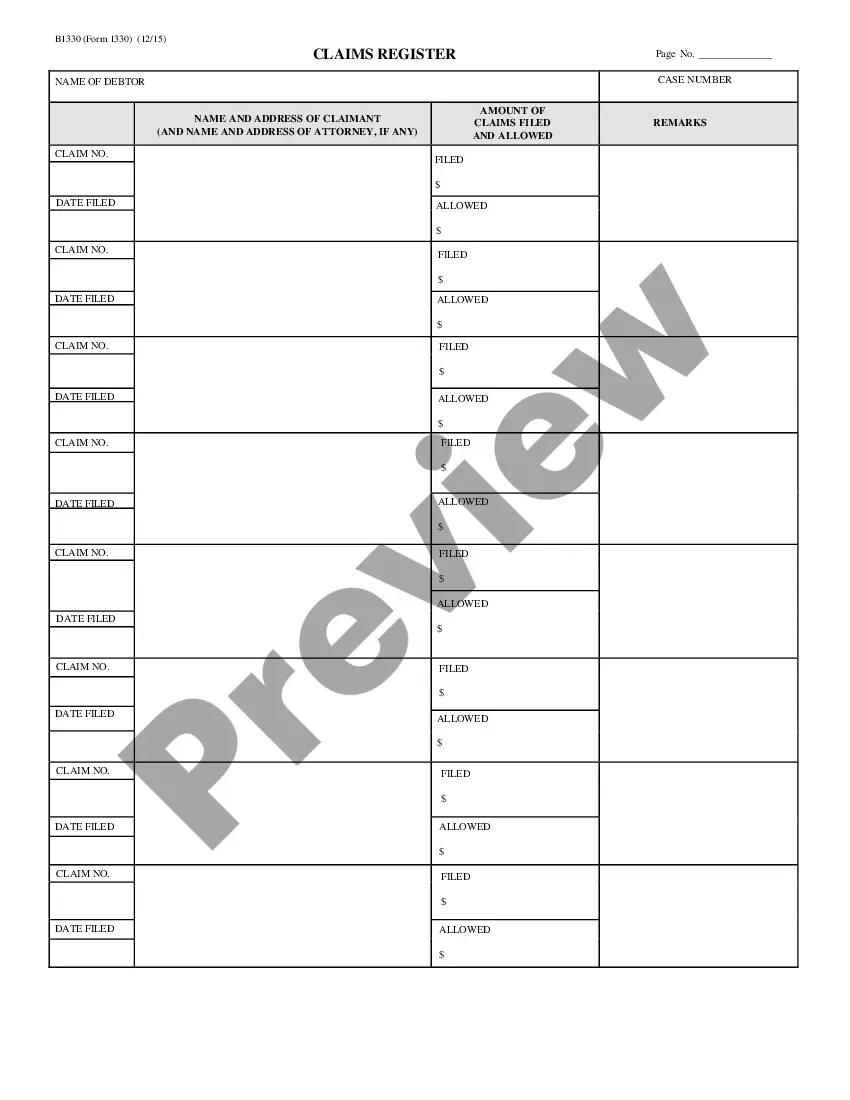
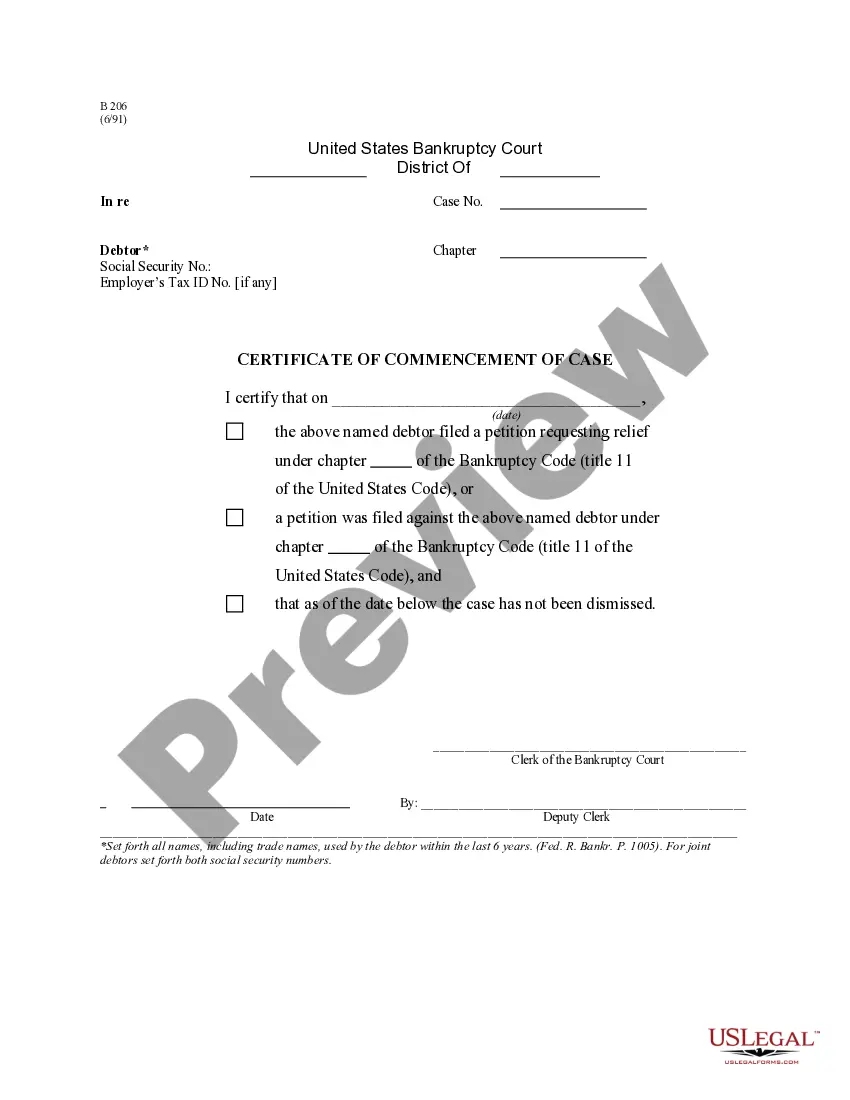
Indiana Claims Register - B 133
Description
How to fill out Claims Register - B 133?
Choosing the right legitimate document design could be a have difficulties. Obviously, there are a lot of layouts accessible on the Internet, but how do you get the legitimate develop you want? Use the US Legal Forms internet site. The support delivers thousands of layouts, for example the Indiana Claims Register - B 133, that you can use for business and personal requirements. Every one of the kinds are inspected by professionals and meet state and federal demands.
If you are presently signed up, log in for your account and then click the Obtain option to have the Indiana Claims Register - B 133. Use your account to check throughout the legitimate kinds you might have ordered previously. Proceed to the My Forms tab of your respective account and have one more duplicate of your document you want.
If you are a whole new consumer of US Legal Forms, here are simple guidelines that you should stick to:
- First, make certain you have selected the right develop for your area/state. You may look over the shape using the Review option and study the shape outline to make certain this is the best for you.
- In case the develop will not meet your expectations, utilize the Seach industry to find the proper develop.
- When you are certain that the shape would work, click on the Buy now option to have the develop.
- Select the rates strategy you need and enter the necessary information. Make your account and buy the transaction making use of your PayPal account or bank card.
- Select the submit format and obtain the legitimate document design for your gadget.
- Comprehensive, modify and printing and indicator the attained Indiana Claims Register - B 133.
US Legal Forms will be the biggest library of legitimate kinds that you can find various document layouts. Use the service to obtain professionally-made files that stick to state demands.
Form popularity
FAQ
Confirm or update basic information like addresses, phone numbers, employer, and insurance plan at every patient encounter. Verify eligibility and authorization before the date of service ? These steps are critical for submitting clean claims yet account for about a quarter of all denials.
Modifier 51 is defined as multiple surgeries/procedures. Multiple surgeries performed on the same day, during the same surgical session. Diagnostic Imaging Services subject to the Multiple Procedure Payment Reduction that are provided on the same day, during the same session by the same provider.
Medicare claim process You present your Medicare ID card to your health care provider. Your provider sends your claim to Medicare. Medicare pays first and sends payment directly to the provider. Medicare sends you a statement saying what you owe. You pay the balance to the provider directly.
Under certain circumstances, it may be necessary to indicate that a procedure or service is significantly greater than usually required.
Claims scrubbing or Claims submission process involves reviewing the claim data before submitting the claims to payers. We utilize the functionality in the practice management systems to check the data integrity. We identify and correct the rejections and work edits before onward submission to insurance payers.
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
Section 50 of the Medicare Claims Processing Manual establishes the standards for use by providers and suppliers (including laboratories) in implementing the Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131.
What Is the Medicare Claims Processing Manual? The CMS Claims Processing Manual is part of the Internet-Only Manual (IOM) repository, which provides access to comprehensive information about CMS-administered programming.