Idaho Qualifying Event Notice Information for Employer to Plan Administrator
Instant download
Description
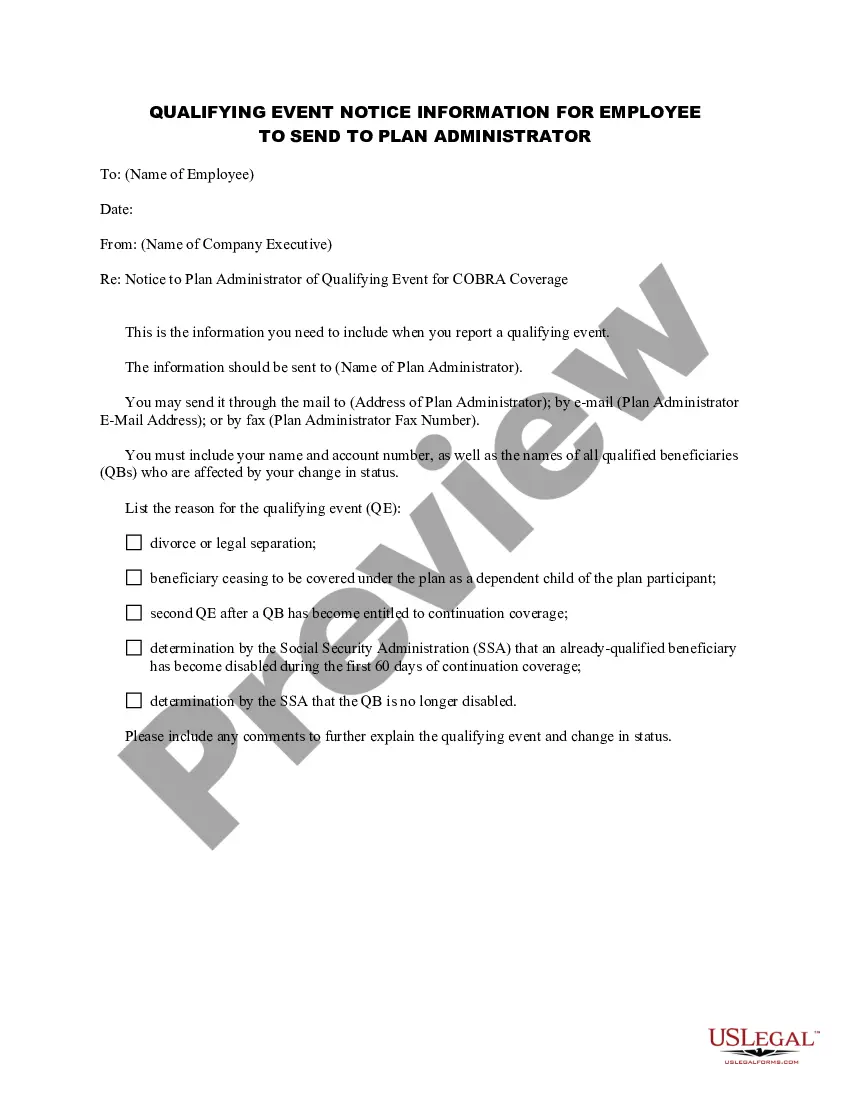
This AHI form is a Notice to Plan Administrator of Qualifying Event for COBRA Coverage.
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
If you need to compile, obtain, or create sanctioned document templates, utilize US Legal Forms, the largest collection of legal documents available online.
Make use of the website's user-friendly and efficient search feature to locate the documents you require.
Numerous templates for business and personal purposes are organized by categories and states, or keywords.
Step 4. Once you have found the form you need, click the Purchase now button. Choose the pricing plan you prefer and enter your details to register for an account.
Step 5. Complete the transaction. You may use your credit card or PayPal account to finalize the purchase.
- Employ US Legal Forms to find the Idaho Qualifying Event Notification Details for Employer to Plan Administrator in just a few clicks.
- If you are already a US Legal Forms customer, Log Into your account and then click the Download button to access the Idaho Qualifying Event Notification Details for Employer to Plan Administrator.
- You can also retrieve forms you have previously obtained in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the steps below.
- Step 1. Ensure you have selected the correct form for your city/state.
- Step 2. Use the Preview option to review the form’s details. Remember to check the information.
- Step 3. If you are not satisfied with the form, use the Search field at the top of the screen to find alternative versions of the legal document template.