Colorado Individual Notice of Preexisting Condition Exclusion
Description
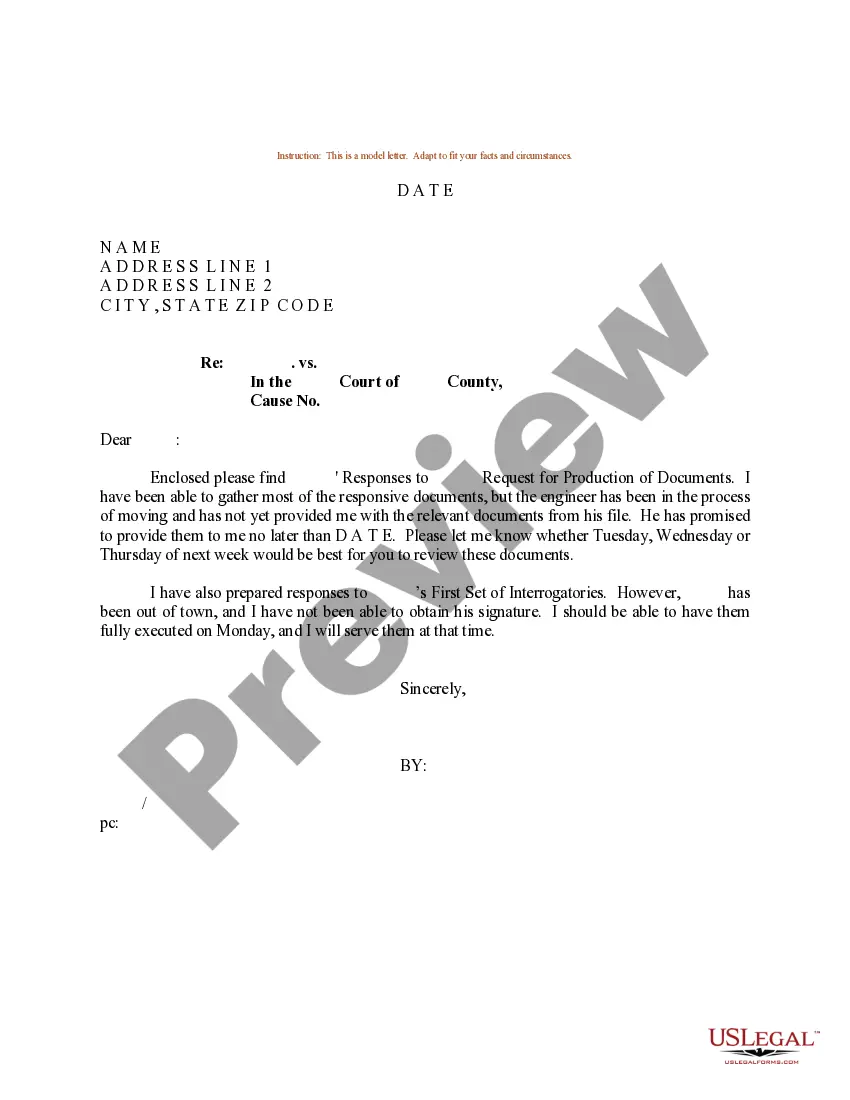
How to fill out Individual Notice Of Preexisting Condition Exclusion?
You can spend numerous hours online seeking the valid document template that meets the state and federal requirements you need.
US Legal Forms provides thousands of valid forms that can be evaluated by experts.
It is easy to download or print the Colorado Individual Notice of Preexisting Condition Exclusion from the service.
If accessible, use the Preview button to view the document template as well.
- If you already have a US Legal Forms account, you can sign in and click on the Download button.
- Next, you can complete, modify, print, or sign the Colorado Individual Notice of Preexisting Condition Exclusion.
- Every valid document template you obtain is yours indefinitely.
- To acquire an additional copy of any purchased form, visit the My documents section and click on the respective button.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure that you have selected the correct document template for the state/city you choose.
- Review the form details to confirm that you have selected the right template.
Form popularity
FAQ
Clinical Nurse Specialist, Kay Greveson, explains: A pre-existing medical condition can be affected by changes in temperature and climate and should always be declared, even if it is being controlled by medication.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.