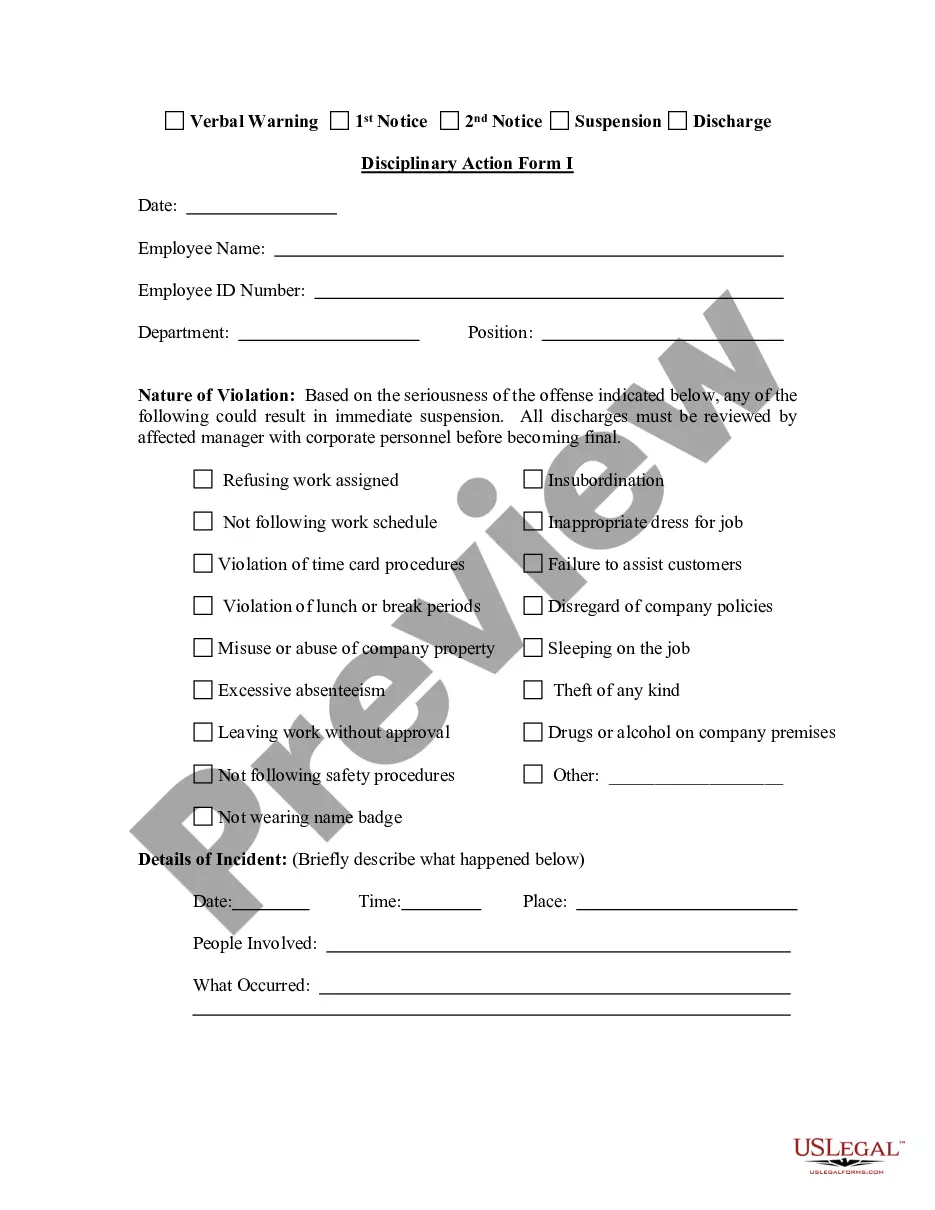
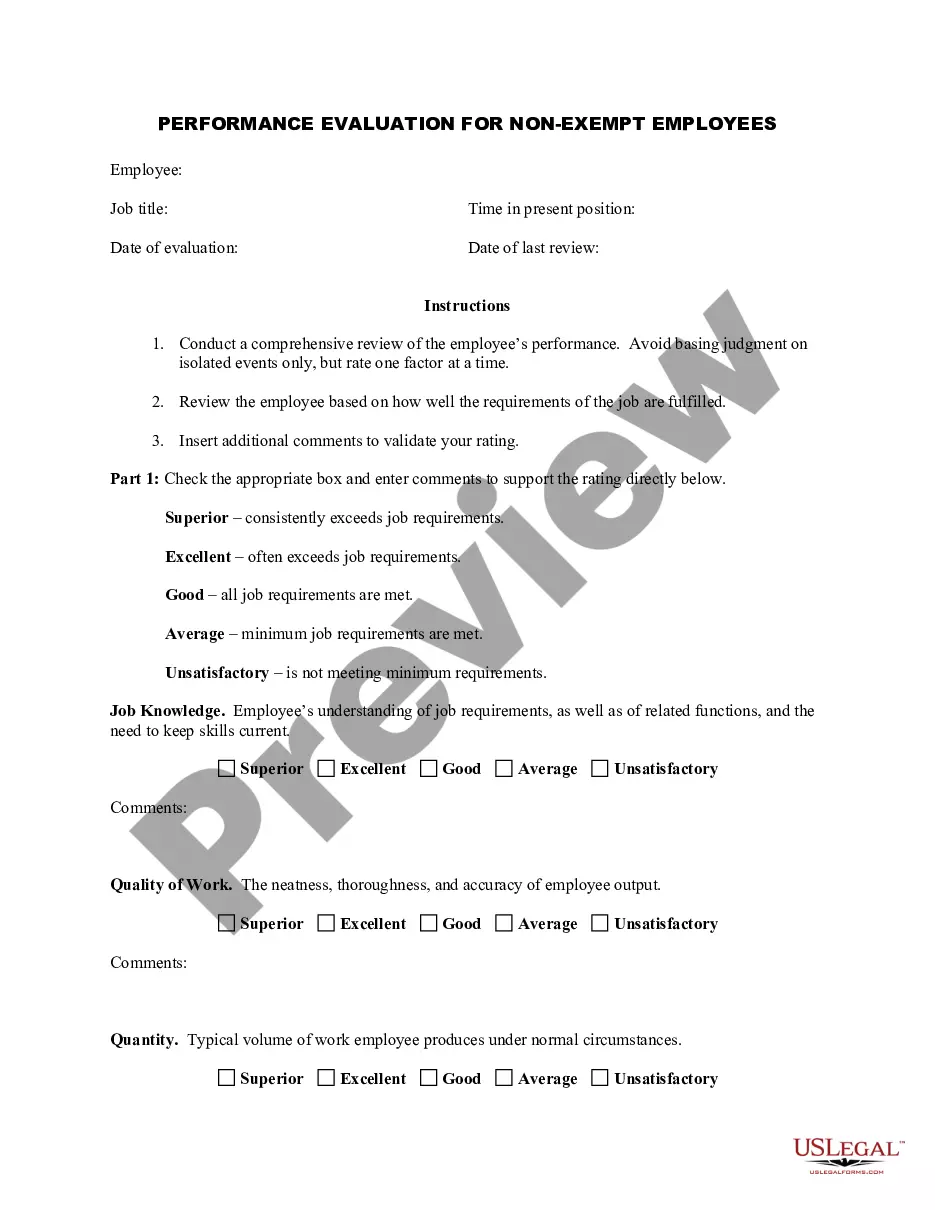
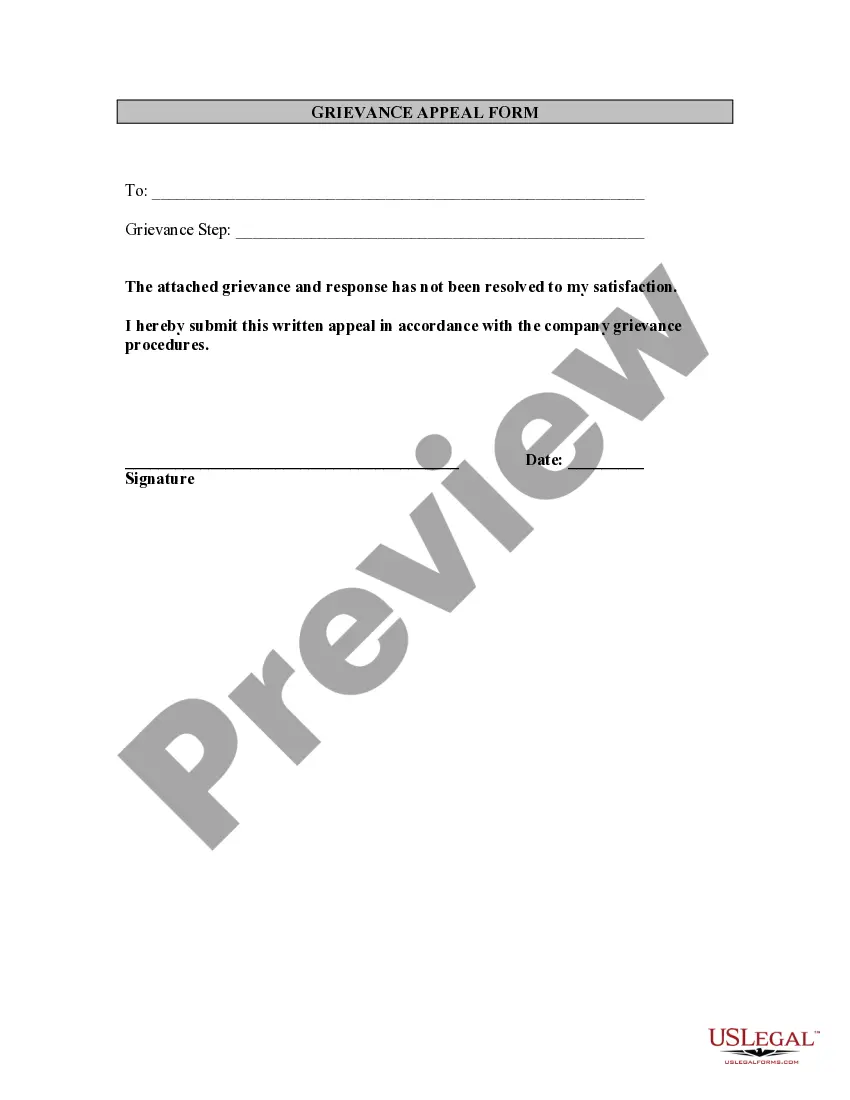
Arizona Employee Grievance Appeal Form
Description
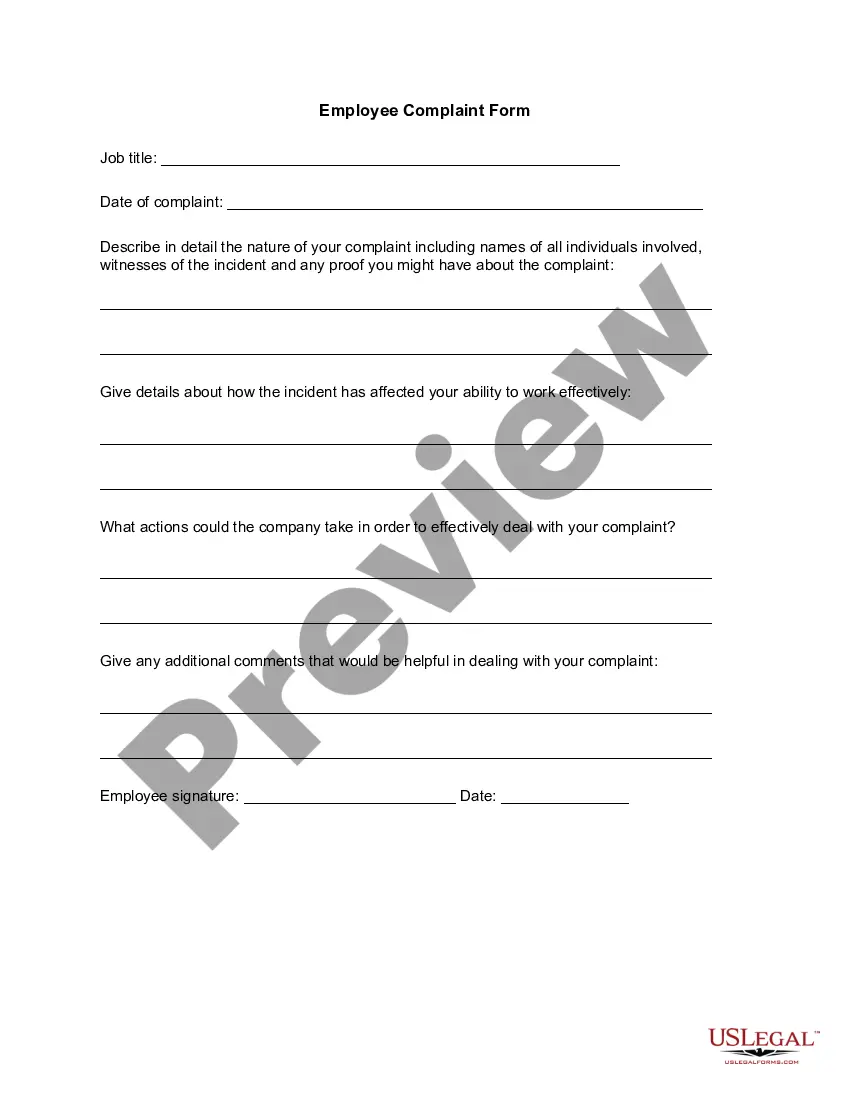
How to fill out Employee Grievance Appeal Form?
You might spend countless hours online attempting to locate the authentic document format that aligns with the federal and state requirements you need.
US Legal Forms offers a vast array of authentic forms that have been assessed by professionals.
You can conveniently obtain or print the Arizona Employee Grievance Appeal Form from our service.
If available, utilize the Review button to browse through the document format as well.
- If you already possess a US Legal Forms account, you can Log In and click the Acquire button.
- Subsequently, you can complete, modify, print, or sign the Arizona Employee Grievance Appeal Form.
- Every authentic document format you acquire is yours permanently.
- To retrieve another copy of any purchased form, navigate to the My documents tab and click the corresponding button.
- If you are using the US Legal Forms website for the first time, follow the straightforward instructions outlined below.
- Initially, ensure that you have selected the appropriate document format for your state/city of choice.
- Review the form details to verify that you have chosen the correct form.
Form popularity
FAQ
Providers must understand The Health Plan grievance system in order to assist members who wish to utilize a grievance system process....Specifically, The Health Plan adheres to the following grievance resolution process:Acknowledgement.Communication and Information.Resolution.Decision making.
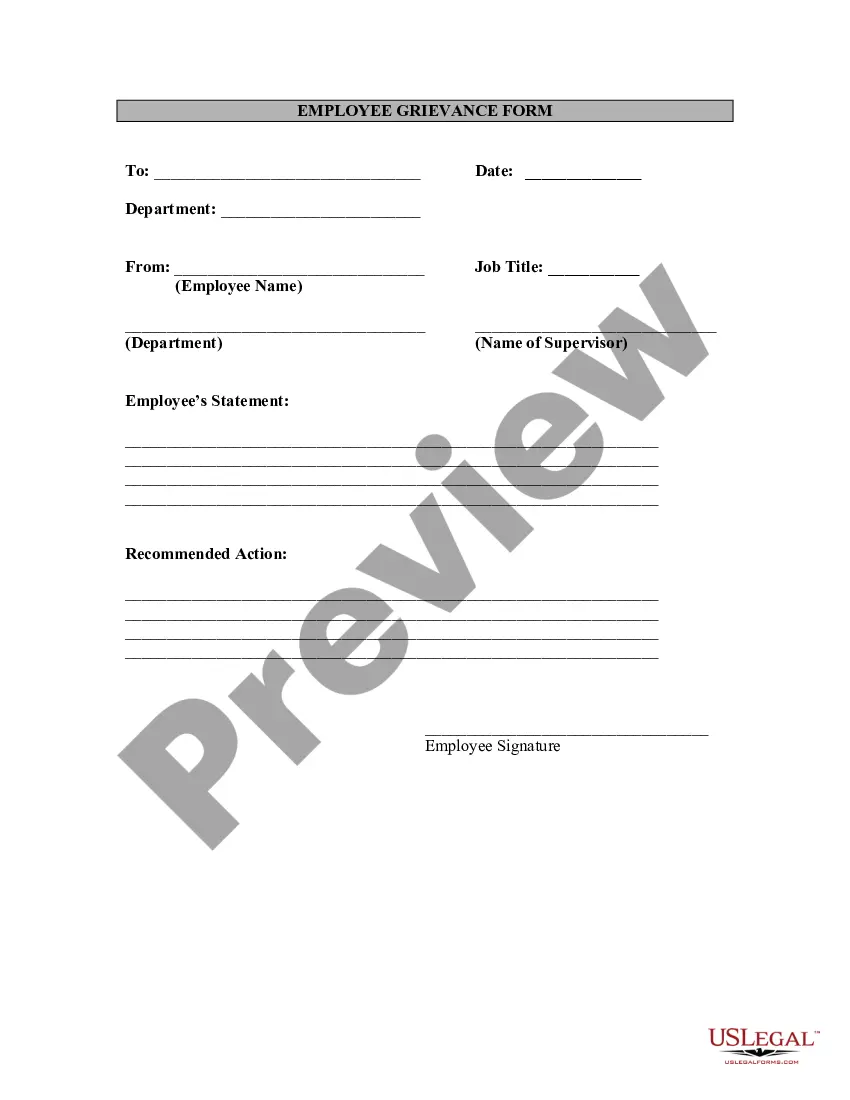
Grievance: Concerns that do not involve an initial determination (i.e. Accessibility/Timeliness of appointments, Quality of Service, MA Staff, etc.) Appeal: Written disputes or concerns about initial determinations; primarily concerns related to denial of services or payment for services.
6. DWIHN has 72 hours from the receipt of the expedited MI Health Link first level request to review and make a determination and within 30 calendar days from receipt of the non-expedited MI Health Link first level internal/local appeal request to the enrollee.
Second opinions involve an independent review of all of the data by a multidisciplinary team. It is not uncommon for the review of the biopsy or surgical slides to lead to a change in the diagnosis. This may then lead to a change in the recommended treatment.
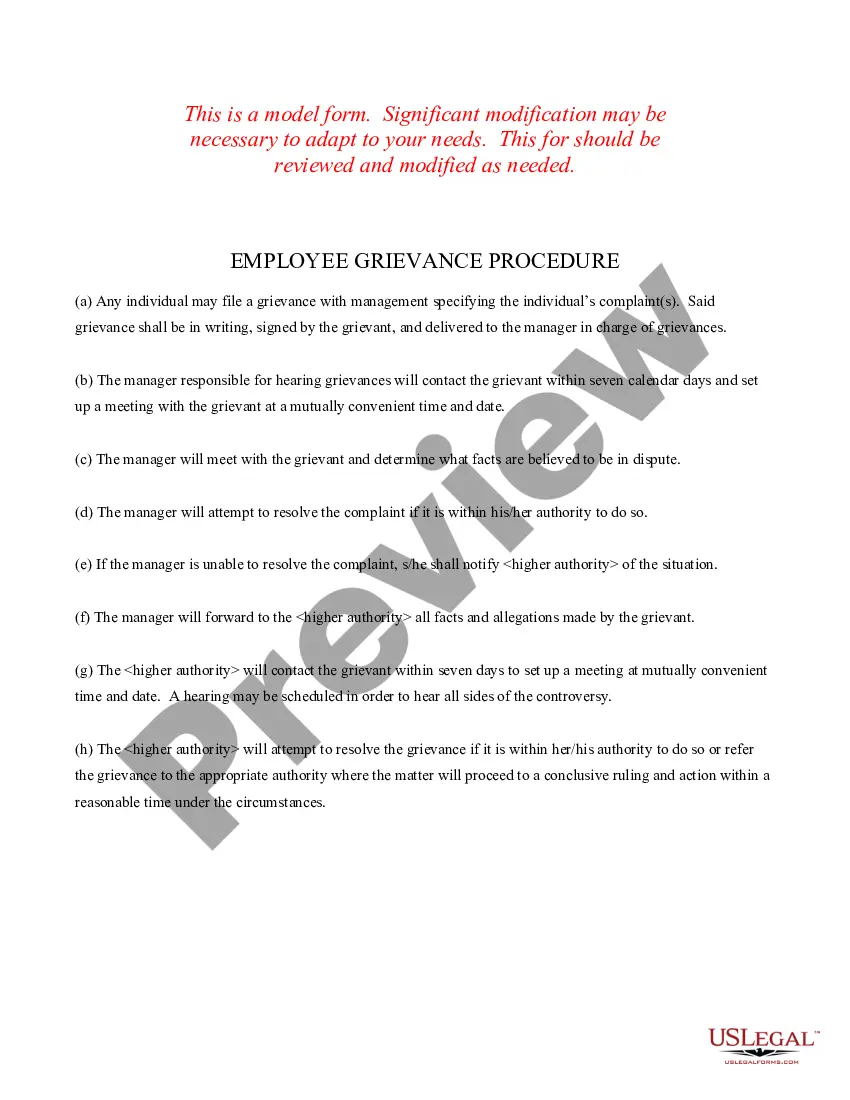
Step 1 - raise the issue informally with the employer. Step 2 raise the issue formally with a grievance letter. Step 3 - grievance investigation should take place. Step 4 - a grievance hearing may be required to review the evidence and for a decision to be made.
Further discussion will likely occur, and if management and the union cannot come to an agreement, the dispute will normally be brought to a national union officer, who will work with management to try and resolve the issue.
The ninety (90) day time frame may be extended up to fourteen (14) days should the consumer or legal representative request an extension or if additional info is needed.
An adverse benefit determination can deny, terminate, suspend or reduce your services. If an inpatient behavioral health hospitalization request is denied. An expedited appeal request must be in writing. An advanced notice must be included each time an IPOS is developed.
Steps to solve a grievanceStep 1: Study the problem.Step 2: Work out possible solutions.Step 3: Rate your choices.Step 4: State the grievance clearly and prepare carefully.Step 5: Present the grievance to management.Step 6: Getting the first response.Step 7: Taking the matter further.Step 8: Declaring a dispute.More items...?
Local Appeal This is a process where you, your guardian, parent or legal representative may request a review of the decision to deny, suspend, reduce or terminate a Medicaid covered service. With your written consent, your provider may also file an appeal on your behalf.