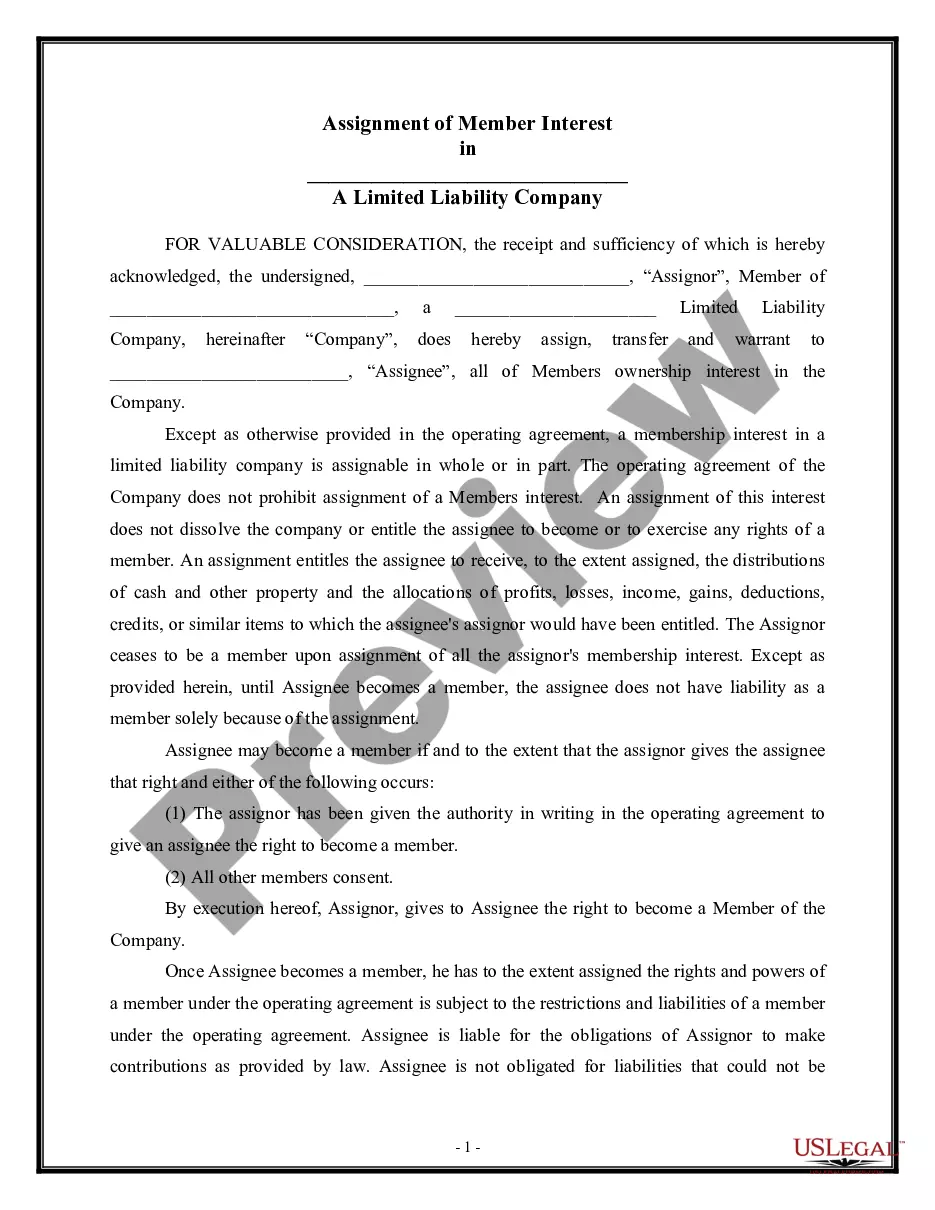
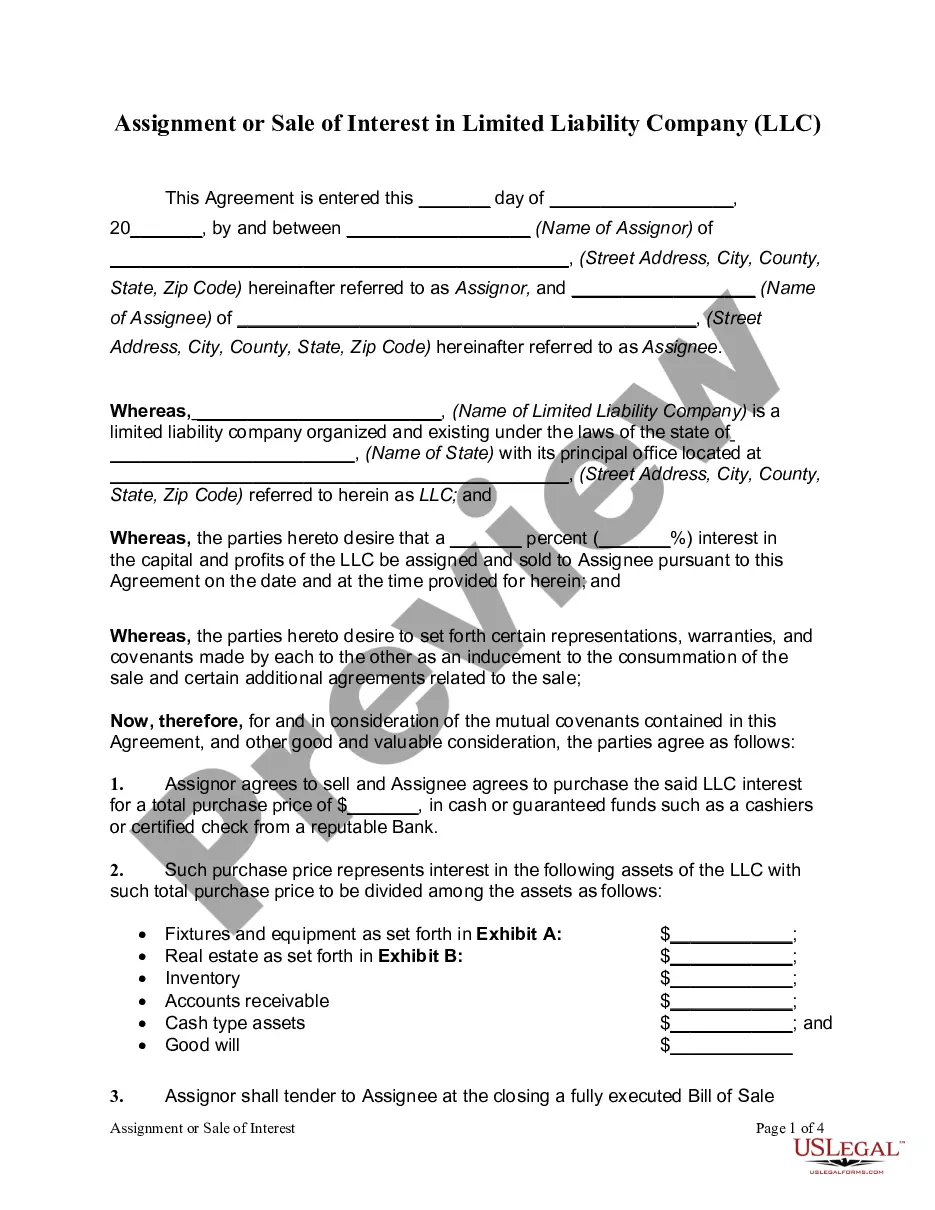
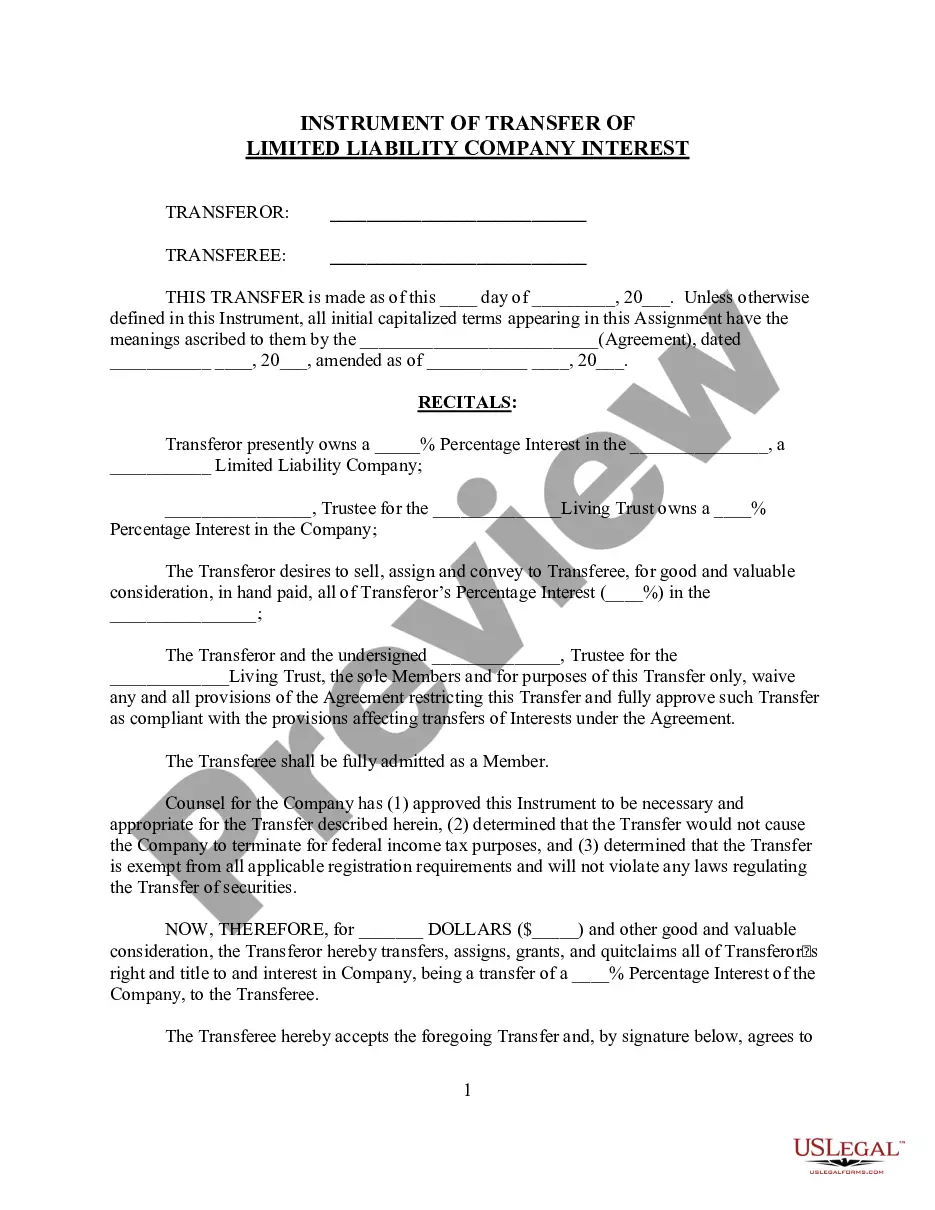
Member Liability Llc Statement With Text
Description
How to fill out Assignment Of Member Interest In Limited Liability Company - LLC?
Regardless of whether for corporate objectives or personal issues, everyone encounters legal matters at some stage in their lives.
Filling out legal documents necessitates meticulous consideration, starting from selecting the appropriate form template. For instance, if you opt for an incorrect version of a Member Liability Llc Statement With Text, it will be denied upon submission. Thus, it is critical to have a reliable source of legal forms like US Legal Forms.
With an extensive library of US Legal Forms, you do not need to waste time searching for the appropriate template online. Utilize the library’s straightforward navigation to find the right form for any scenario.
- Locate the template you require by utilizing the search bar or browsing the catalog.
- Review the form’s description to ensure it aligns with your situation, state, and county.
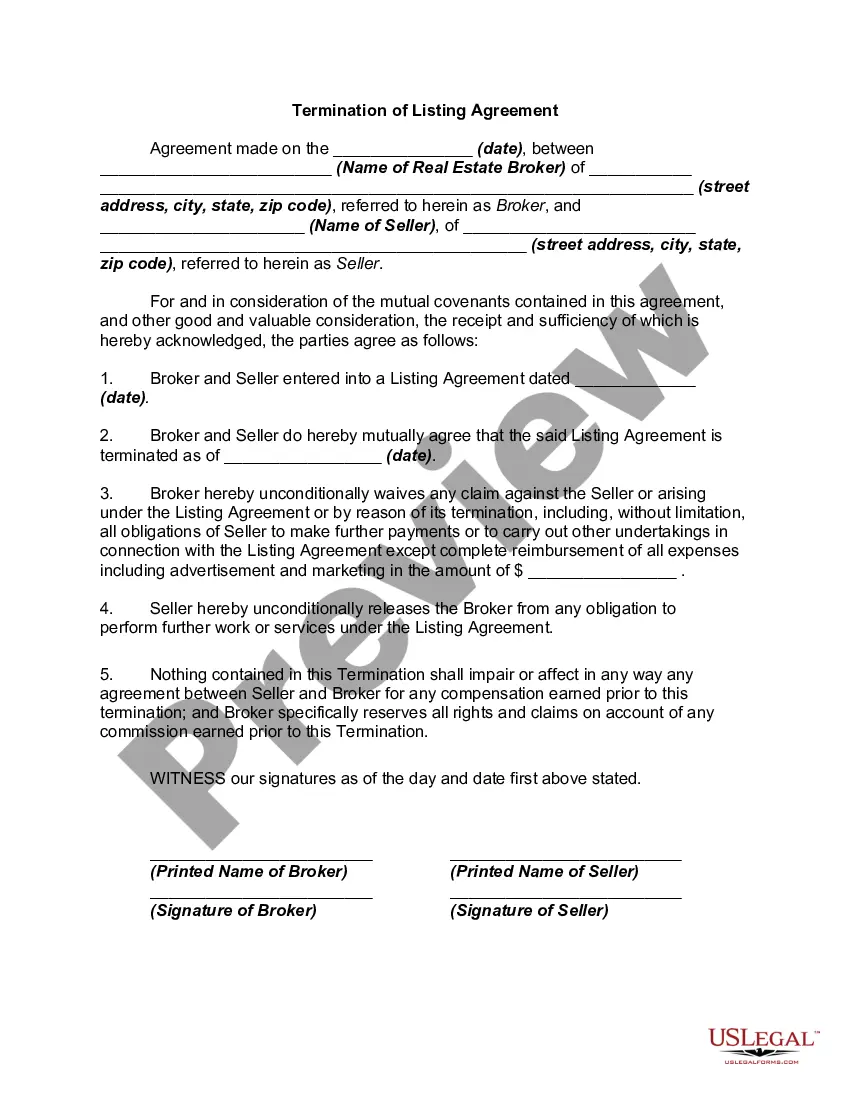
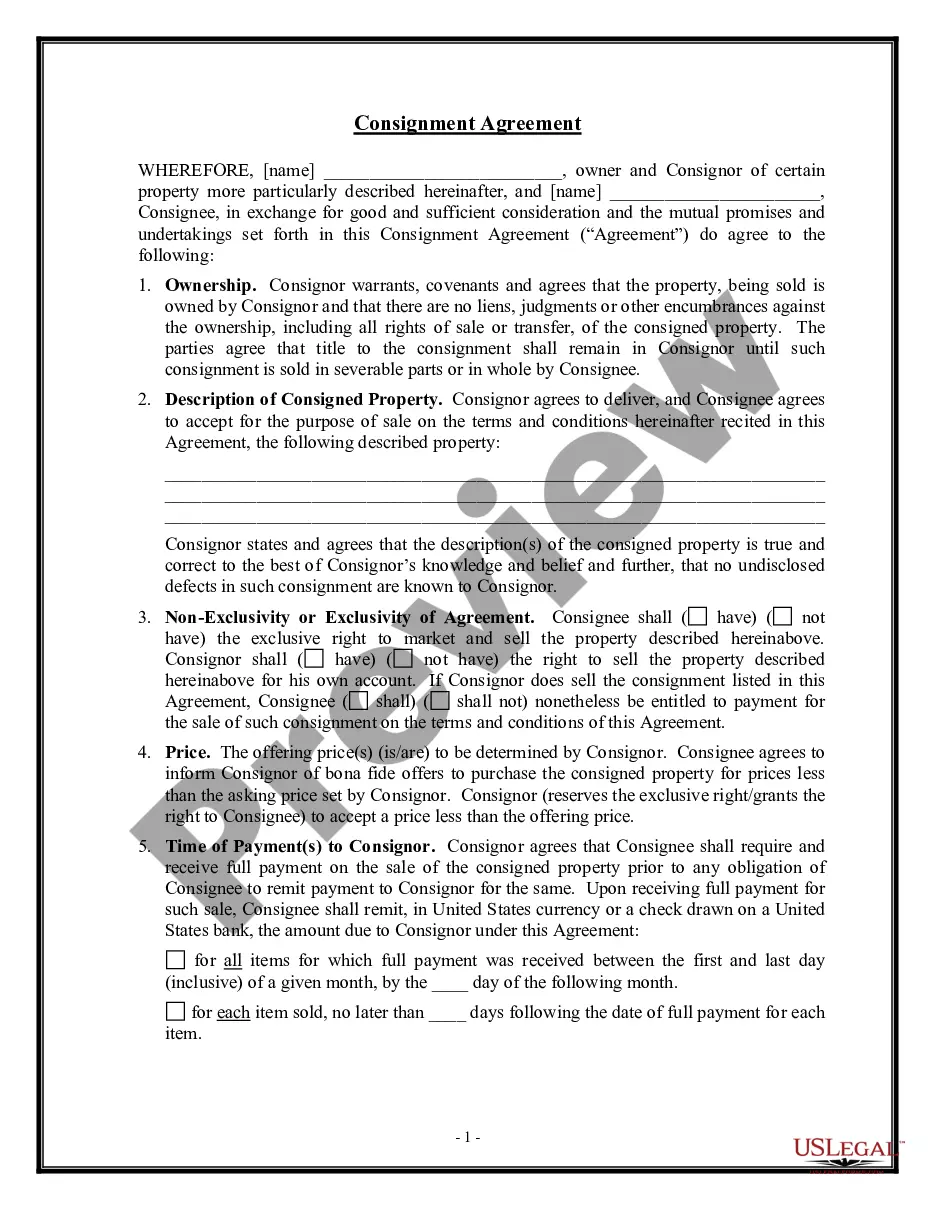
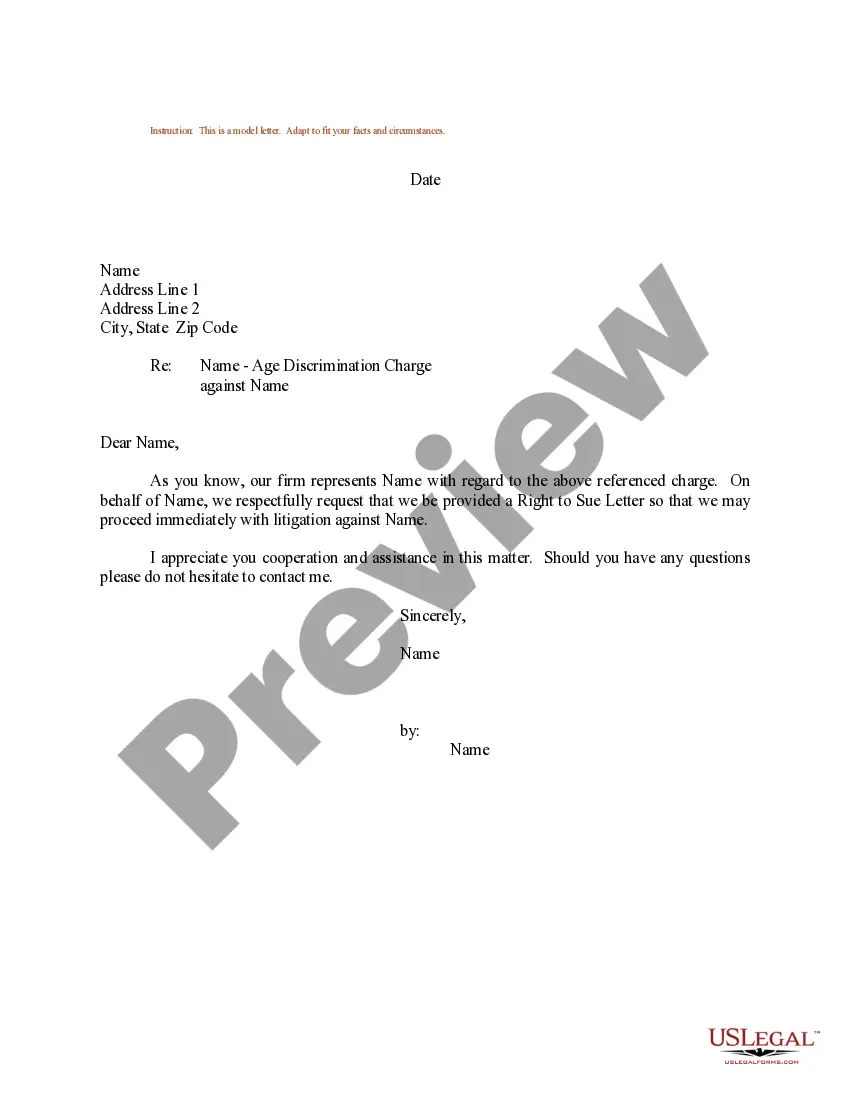
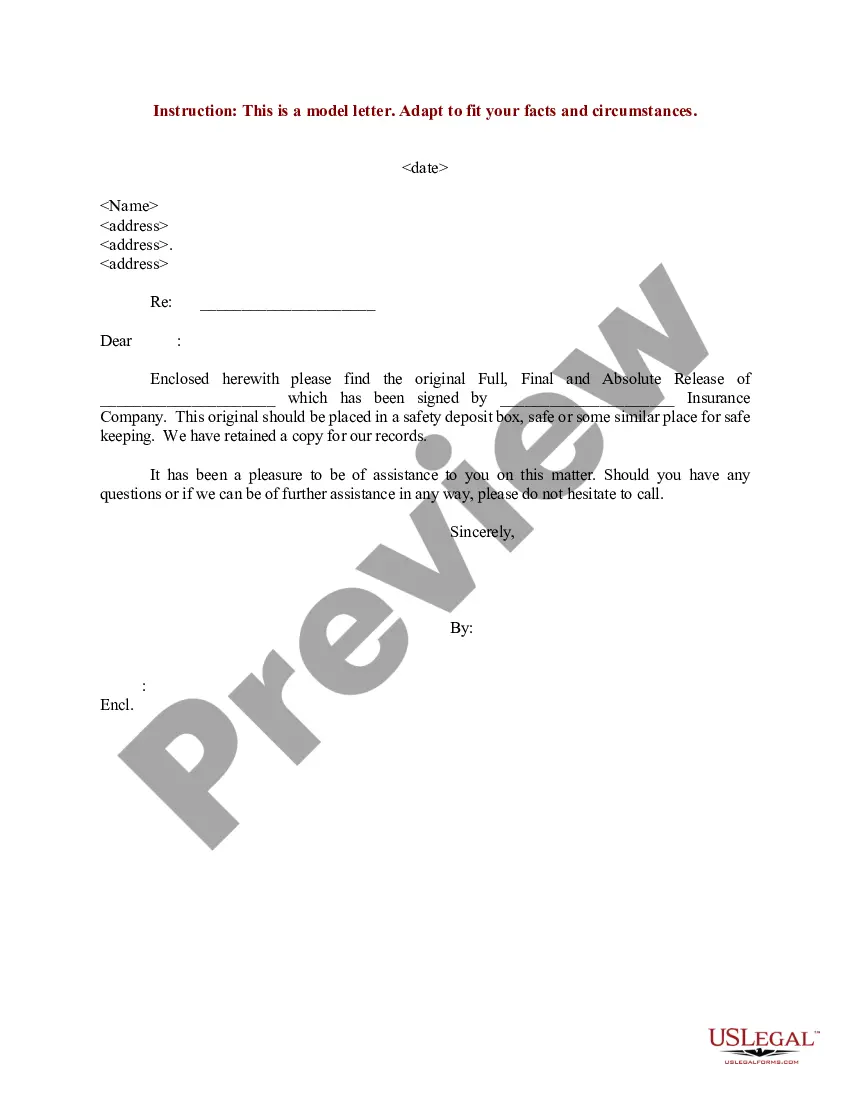
- Click on the form’s preview to analyze it.
- If it is the incorrect form, return to the search tool to find the Member Liability Llc Statement With Text template you seek.
- Obtain the template when it fulfills your specifications.
- If you possess a US Legal Forms account, click Log in to access previously saved documents in My documents.
- If you have yet to create an account, you can download the form by clicking Buy now.
- Select the relevant pricing option.
- Complete the account registration form.
- Choose your payment method: utilize a credit card or PayPal account.
- Select the document format you wish and download the Member Liability Llc Statement With Text.
- Once it is saved, you can fill out the form using editing software or print it and complete it by hand.
Form popularity
FAQ
Other examples of utilization reviews might include determining whether or not a patient should be transferred to a specialty trauma ICU at a regional center or getting insurance approval for an extended hospital stay that goes beyond the typical guidelines.
File an Application for Reinstatement for a business and pay the fee online. The filing fee is $70. An online service fee may be added to the filing fee. Print and Mail the Application for Reinstement.
Types of Utilization Management UM has three main types of reviews: prospective, concurrent, and retrospective.
Utilization Review (UR) is the evaluation of medical care services for the treatment provided to an injured worker.
To receive a tax clearance certificate when shutting down a business, a business must file all returns to date and a final franchise and excise tax return through the date of liquidation or the date on which the business ceased operations in Tennessee.
Your Personal Info Social Security Number. Driver's License Number. Address. Telephone Number. Valid email address. Tennessee Unemployment Insurance claimants receive their benefits via the Tennessee Automated Payment (TAP) debit card or direct deposit. ... DD 214 Member 4 if you served in the military in the past 18 months.
Utilization review nurses perform frequent case reviews, check medical records, speak with patients and care providers regarding treatment, and respond to the plan of care. They also make recommendations regarding the appropriateness of care for identified diagnoses based on the research results for those conditions.
Summary. Utilization review is a process designed to ensure that medical care is effective, efficient, and in line with evidence-based standards of care. Utilization review specialists are often nurses. They work for health insurance companies, hospitals, and various other medical providers.