Cobra Enrollment Form With Dependent Data
Description
How to fill out Cobra Enrollment Form With Dependent Data?
Individuals often connect legal documentation with complexity that requires a specialist's intervention.
In a sense, this is accurate, as creating the Cobra Enrollment Form With Dependent Data necessitates considerable knowledge of specific subject matters, including both state and local laws.
Nevertheless, with US Legal Forms, the process has become more straightforward: a comprehensive online library containing ready-to-use legal documents for any personal or business situation tailored to state legislation is now accessible to everyone.
Print your file or upload it to an online editor for quicker completion. Every template in our library is reusable: once obtained, they remain saved in your account. You can access them anytime you need through the My documents tab. Discover all the benefits of utilizing the US Legal Forms platform. Sign up today!
- US Legal Forms provides over 85k current documents categorized by state and area of application, allowing you to find the Cobra Enrollment Form With Dependent Data or any other specific template in just minutes.
- Users with existing accounts and active subscriptions need to Log In and click Download to retrieve the form.
- New users must first register and subscribe before they can save any documents.
- Follow this step-by-step guide to obtain the Cobra Enrollment Form With Dependent Data.
- Review the page content carefully to ensure it satisfies your requirements.
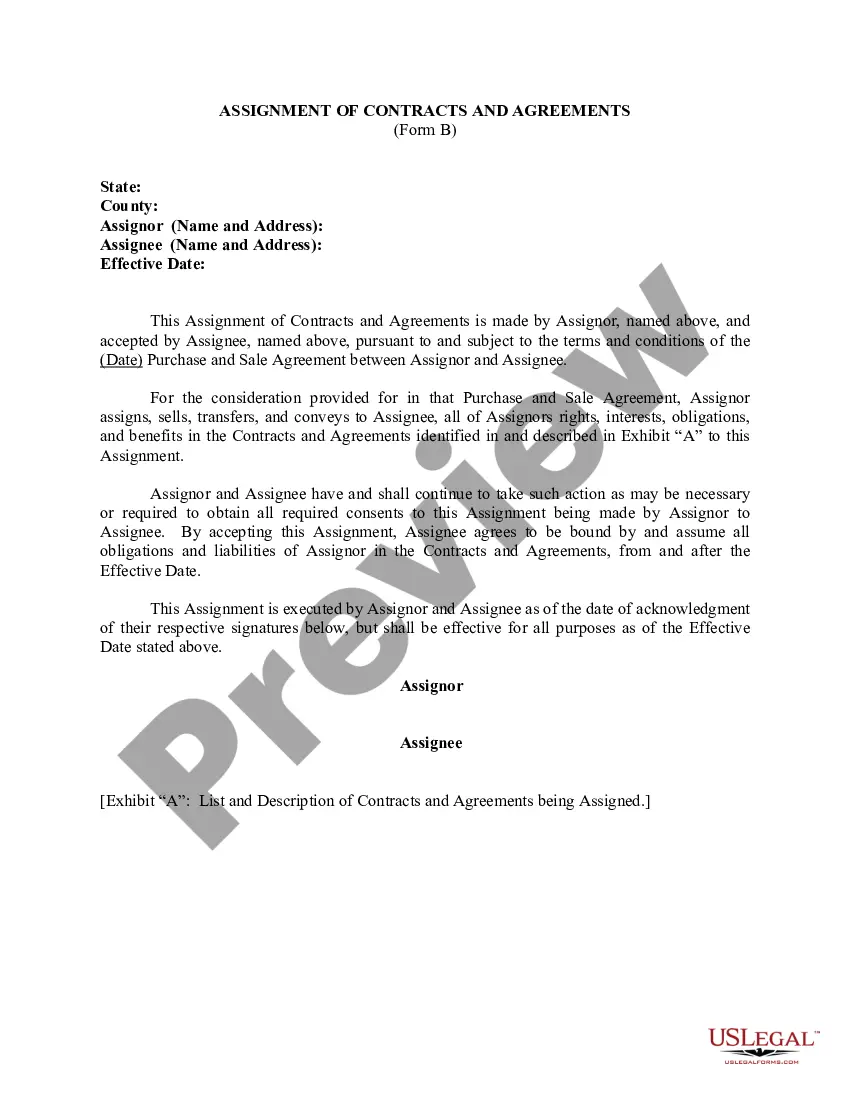
- Check the form description or confirm it using the Preview option.
- If the original form doesn’t meet your criteria, look for another example using the Search field at the top.
- Click Buy Now when you locate the appropriate Cobra Enrollment Form With Dependent Data.
- Select a subscription plan that aligns with your needs and budget.
- Create an account or Log In to proceed to the payment section.
- Complete your subscription payment via PayPal or credit card.
- Choose the format for your document and hit Download.
Form popularity
FAQ
COBRA participants usually can add dependents during open enrollment periods, provided they comply with the plan's guidelines. During this time, you can submit the COBRA enrollment form with dependent data to request the addition of dependents. Be sure to keep an eye on the specific enrollment dates to maximize your benefits. This process allows flexibility in managing your health coverage.
To add dependents to your health insurance, you typically need to contact your insurance provider for guidance. They will instruct you on filling out the appropriate forms, including the COBRA enrollment form with dependent data. Make sure to provide all required information about your dependents and watch for enrollment periods to avoid lapsing in coverage. This ensures your dependents remain protected.
You can add dependents to your COBRA coverage if they meet the eligibility criteria outlined in your original health plan. It's important to complete the necessary COBRA enrollment form with dependent data accurately. Remember to check for any deadlines or specific instructions for adding dependents to your coverage. This is crucial to maintain comprehensive health benefits.
Yes, you can apply for COBRA coverage for just a dependent if they qualify under your health plan. This usually occurs when the employee experiences a qualifying event, such as job loss or reduction in hours. You must provide the correct details in the COBRA enrollment form with dependent data to ensure proper coverage. This option protects your dependent's health care needs.
To add a dependent to COBRA, you must first review your existing COBRA enrollment. Then, complete the COBRA enrollment form with dependent data, including the necessary details of the new dependent. Be mindful of any deadlines for enrolling dependents to avoid gaps in coverage. This process allows you to extend vital health benefits to your loved ones.
Yes, a dependent can obtain COBRA coverage independently if the employee's health plan covers dependents. However, the dependent must enroll within the required timeframe after the qualifying event. Completing the COBRA enrollment form with dependent data is essential for this process. It ensures that the dependent maintains necessary health insurance coverage.
COBRA primarily focuses on health insurance coverage rather than dependent care services. While COBRA ensures that dependents can maintain their health insurance after certain events, it does not extend to childcare benefits. Thus, you will need to explore separate options for dependent care outside of your Cobra enrollment form with dependent data. Understanding these distinctions is essential for budgeting and ensuring your family's needs are met effectively.
COBRA outlines several qualifying events that allow individuals to secure coverage. These include job loss, a reduction in work hours, divorce, legal separation, a dependent aging out of coverage, the death of the covered employee, and Medicare eligibility. Each of these events provides an opportunity for enrollees to utilize the Cobra enrollment form with dependent data. It's important to act swiftly following any of these events to ensure coverage continues seamlessly.
Filling out the 1095-C for COBRA participants involves providing accurate information about the coverage offered and the duration of that coverage. The form must reflect details such as the employee's status and dependent coverage, which is important for compliance. A properly completed 1095-C clarifies the situation for COBRA participants, especially when referring to the Cobra enrollment form with dependent data. This form aids in ensuring that all necessary tax information is available for filing.
COBRA allows dependents of employees to maintain health insurance coverage after a qualifying event, like job loss or reduced work hours. Your Cobra enrollment form with dependent data includes sections specifically for adding or maintaining dependents. This option ensures that your family members continue to have access to necessary healthcare. It's vital to file the form promptly to avoid coverage gaps.