Consent Release Information Form Psychologist In Harris
Description
Form popularity
FAQ
HIPAA and psychotherapy notes Generally, process notes cannot be shared with others if the therapist does not wish to share the information in them. On the other hand progress notes—usually with a client's permission—are allowed to be shared with others.
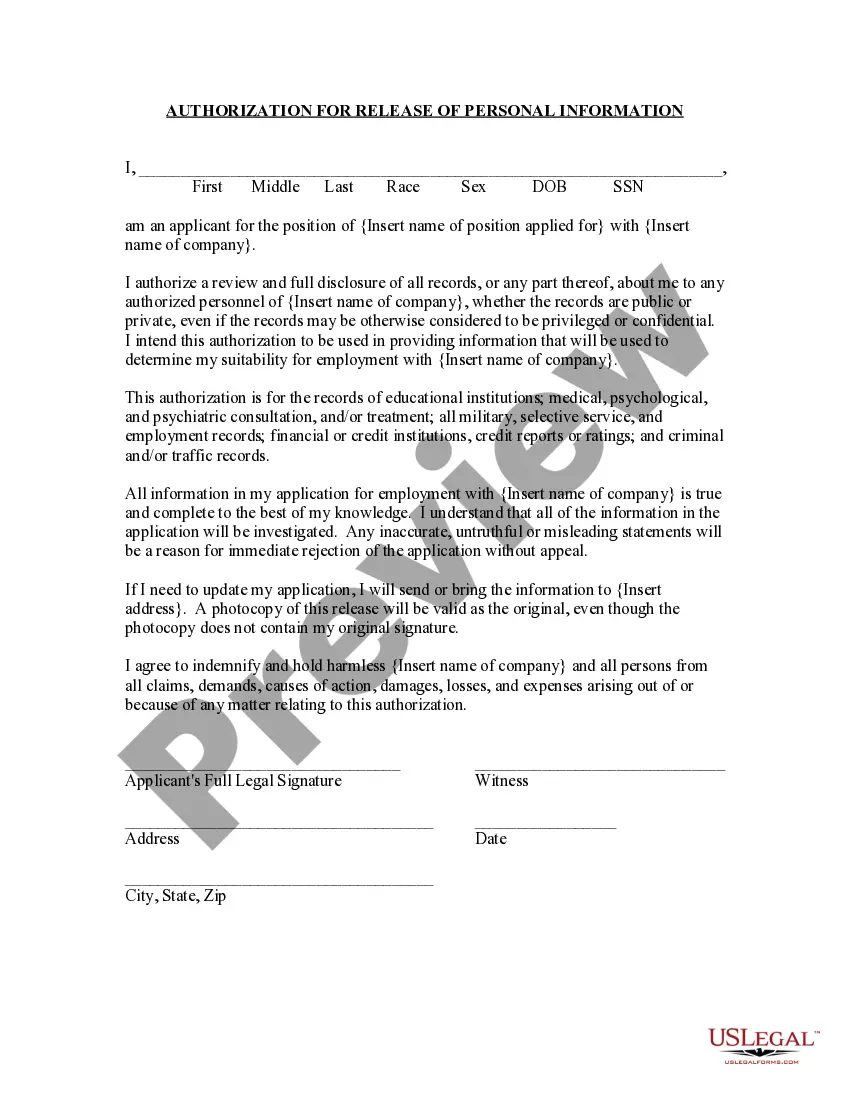
If you are a covered entity, you must comply with HIPAA laws. Under HIPAA, patients have the right to request and receive copies of their medical records, including mental health records. They also have the right to request that their records be corrected if they believe there are errors.
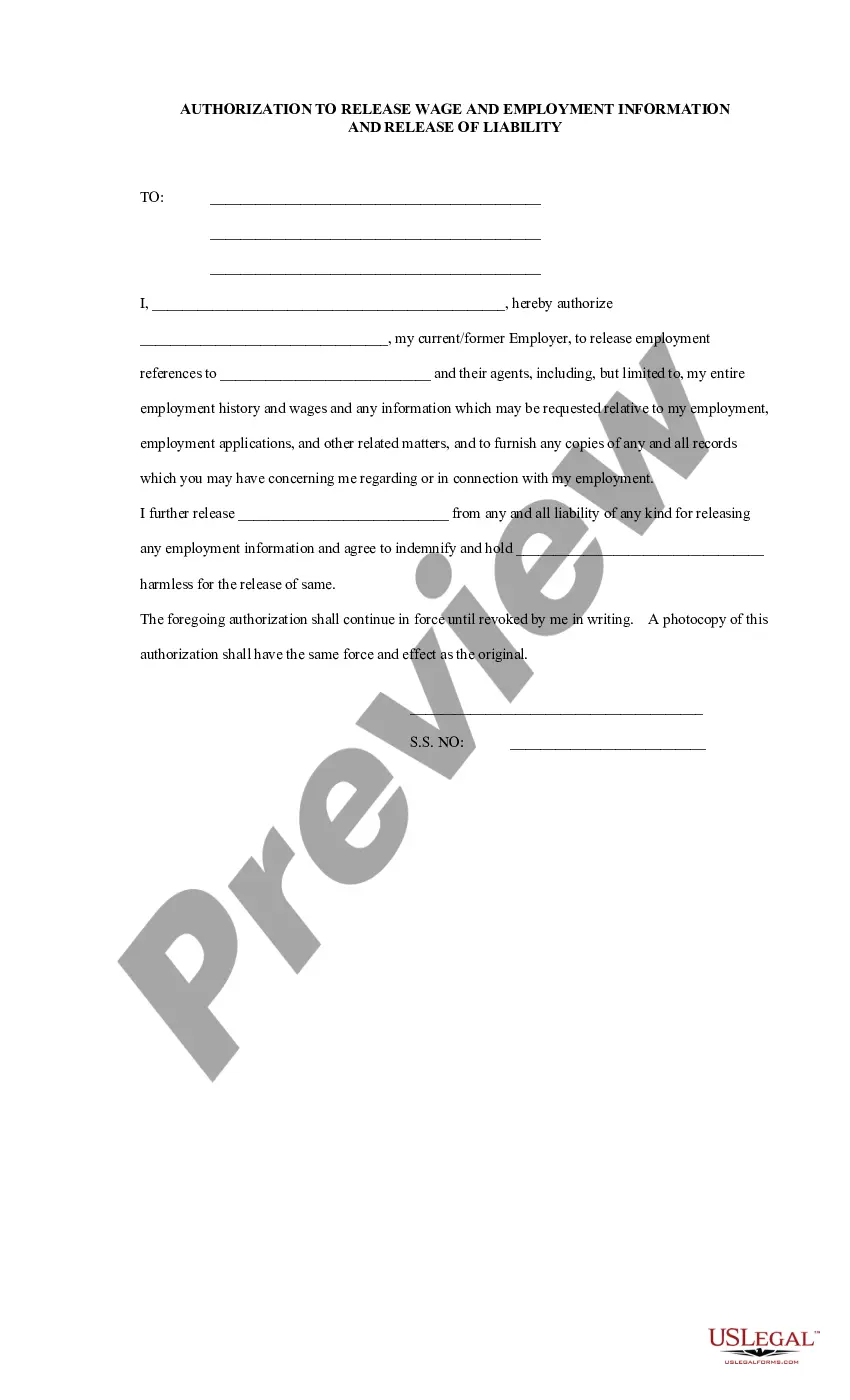
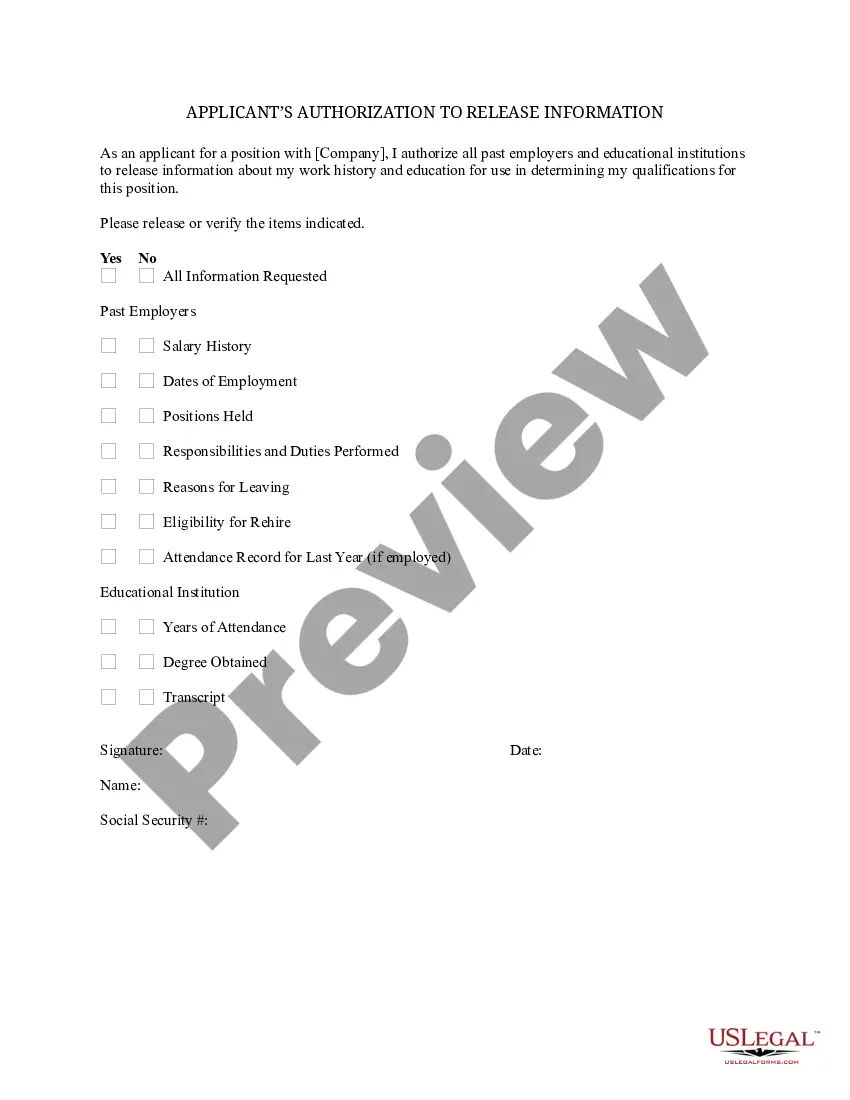
Copies of your healthcare records can be obtained with your written request. To request copies of your medical records complete an authorization form and mail it with a copy of your driver's license to the Health Information Management Department address listed below.
The length of time a therapist will keep records of what you say in therapy sessions will depend on the therapist's practice and state laws. In general, therapists will keep records of sessions for at least seven years.
It's no secret that therapists have to take careful notes during sessions with patients. But did you know that those notes are subject to the same federal privacy laws as other medical records?
Your psychologist will ask questions like whether you've noticed any changes in your sleeping habits, appetite or other behaviors. A psychologist will also want to know what kind of social support you have, so he or she will also ask about your family, friends and coworkers.
The informed consent process should ensure that all critical information about a study is completely disclosed, and that prospective subjects or their legally authorized representatives adequately understand the research so that they can make informed choices.
To obtain informed consent for any treatment or procedure, providers must disclose enough information to enable clients to make informed decisions. This disclosure should include a clear explanation of the risks, their likelihood, as well as the benefits and their likelihood.
There are 4 components of informed consent including decision capacity, documentation of consent, disclosure, and competency. Doctors will give you information about a particular treatment or test in order for you to decide whether or not you wish to undergo a treatment or test.
Informed consent creates a continuing dialogue and promotes a clinician-client relationship that fosters mutual respect, shared decision-making and client autonomy. Informed consent done correctly involves clinicians providing clients with the information necessary to make informed decisions about their treatment.