Here Denied Claim For Primary Eob In Wayne
Description
Form popularity
FAQ
Each time your insurer pays for a service you use, they send you an Explanation of Benefits (EOB). The EOB is your insurance company's written explanation for that claim, showing the name of the provider that covered the service and date(s) of service.
What is the timely filing limit for Oxford appeals? You must submit your claim reconsideration and/or appeal to us within 12 months (or as required by law or your Agreement), from the date of the original EOB or denial.
Denial code CO16 means that the claim received lacks information or contains submission and/or billing error(s) needed for adjudication. In other words, the submitted claim doesn't have what the insurance company wants on it, or something is wrong.
EOB stands for “end of business,” a phrase that has the same meaning as “close of business.” In other words, the time when a company closes its doors at the end of the day.
EOD stands for the end of the business day ing to the sender's time zone. Suppose a client requests a deliverable by EOD. In that case, most companies expect you to deliver by the end of the business day ing to their time zone unless specified otherwise.
Kaiser Permanente has the lowest claim denial rate among major health insurance companies, which the analysis defined as brands offering Marketplace plans in seven states or more during the 2025 plan year. The California-based healthcare company denied just 6% of claims based on the available 2023 data.
Nationwide, high-volume insurers with higher in-network denial rates across HealthCare states included Blue Cross Blue Shield of Alabama (35% for its 12 plans in that state), UnitedHealth Group (33% across 274 plans in 20 states), Health Care Service Corporation (29% across 915 plans in four states), Molina ...
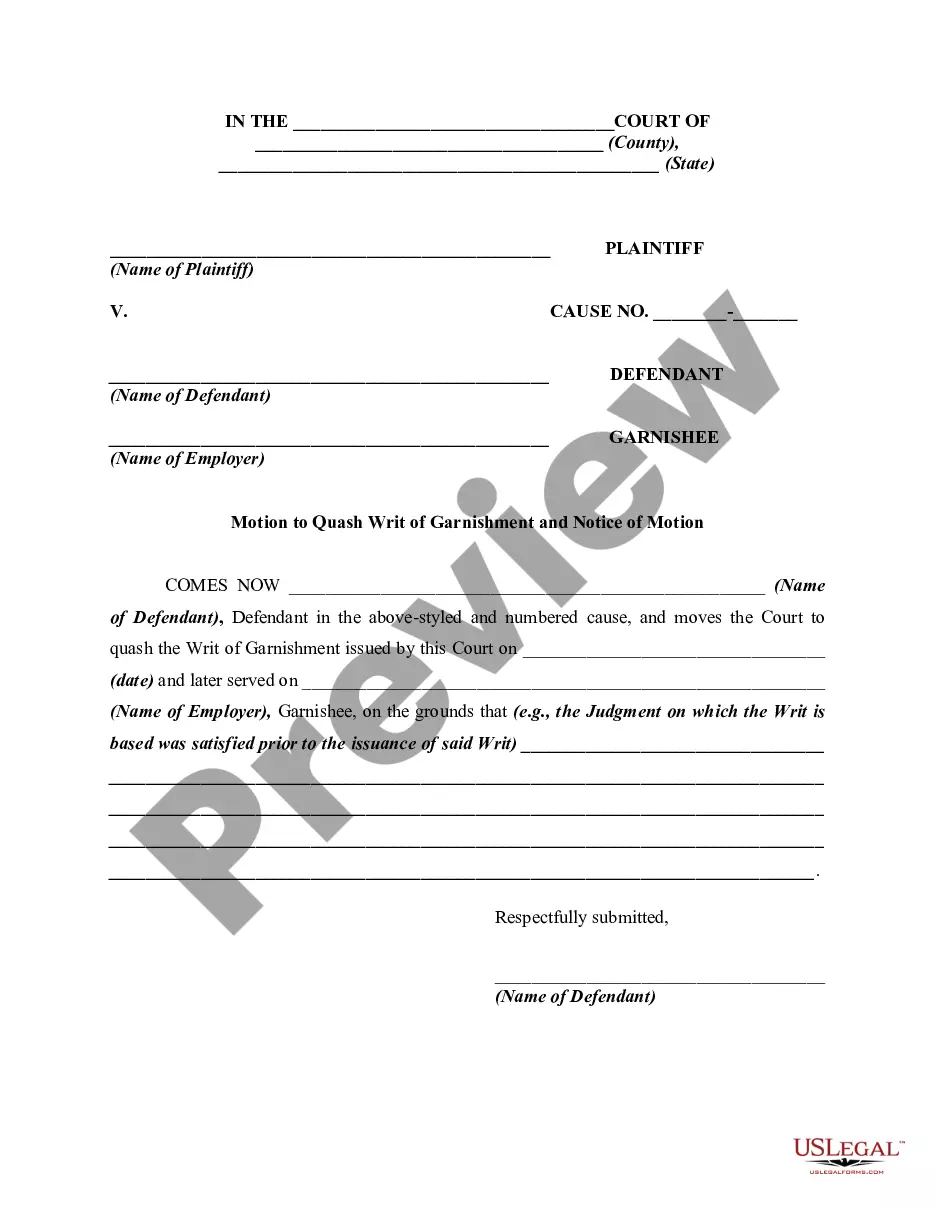
If your resubmitted claim is denied and you believe the denial was improper, you may appeal the decision ing to the carrier's guidelines. Make sure you know exactly what information you need to submit with your appeal. Keep in mind that appeal procedures may vary by insurance company and state law.
Which insurance companies are considered the worst? Allstate. Allstate has provided insurance to Americans since 1931. Progressive. Progressive was launched in 1937. UnitedHealth. Richard T. State Farm. State Farm has been in business since 1922. Elevance Health (formerly Anthem) ... Unum. Federal Employee Benefits. Farmers.
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.