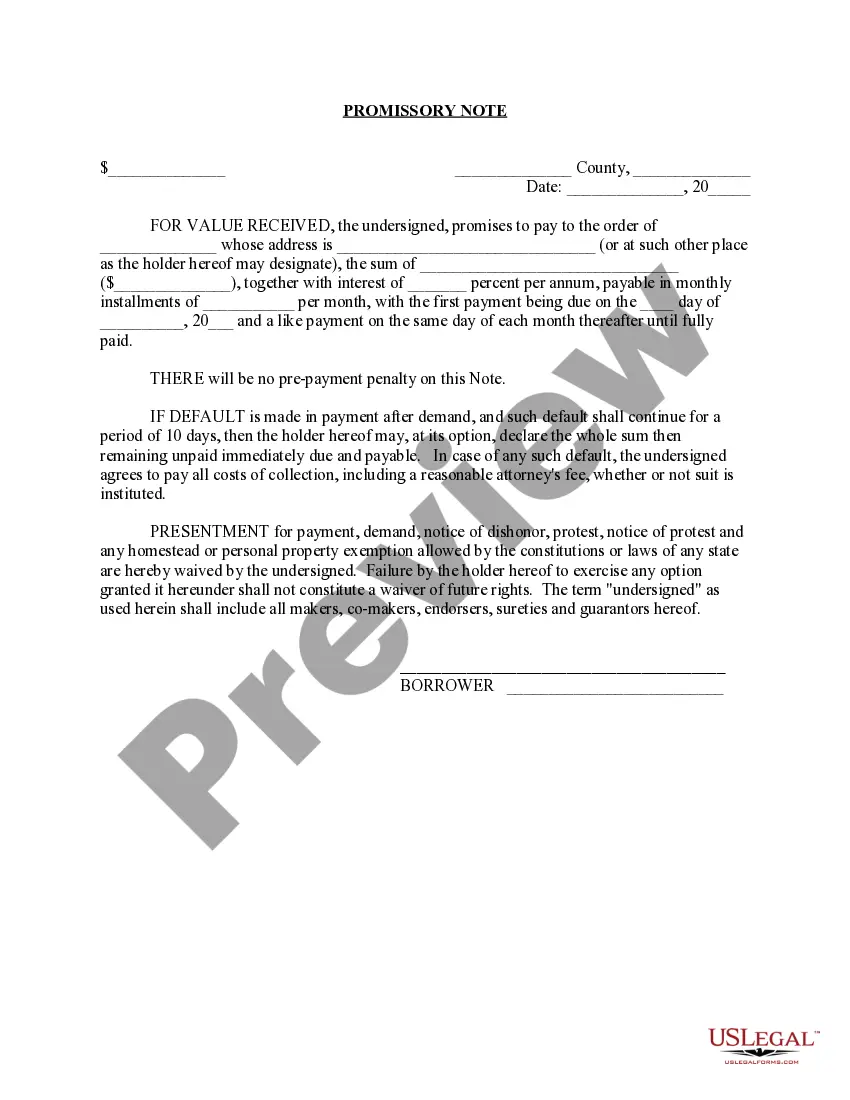
The parties may agree to a different performance. This is called an accord. When the accord is performed, this is called an accord and satisfaction. The original obligation is discharged. In order for there to be an accord and satisfaction, there must be a bona fide dispute; an agreement to settle the dispute; and the performance of the agreement. An example would be settlement of a lawsuit for breach of contract. The parties might settle for less than the amount called for under the contract.
Denied Claim Agreement For Primary Eob In Middlesex
Description
Form popularity
FAQ
Example Sentences However, the federal rule does permit the release of certain information in billing and statements, like an EOB. Bills from three separate departments of the providers system, in amounts that bear no relationship to the preliminary statement or to the EOB's we got.
An Explanation of Benefits (EOB) code corresponds to a printed message about the status or action taken on a claim. Providers will find a list of all EOB codes used with the corresponding description on the last page of the Remittance Advice.
Maintaining accurate documentation and keeping records organized will help you show compliance with filing requirements and will make it more likely that you'll receive a recovery of your denied payments.
You should always save your Explanation of Benefits until you get the final bill from your doctor or health care provider. Insurance companies make it easy for members to view past EOBs online, so there's no need to keep a paper copy if you have an online account.
End of day (EOD), end of business (EOB), close of business (COB), close of play (COP), or end of play (EOP) is the end of the trading day in financial markets, the point when trading ceases.
Incorrect or missing information on the claim form Probably the most common reason that a claim is rejected is simple mistakes on the claim form. This could be in the form of missing or incorrect information. Insurance providers require specific details to assess and process claims accurately.
Claims rejections occur either at the clearinghouse or the payor. It usually happens because of a problem or mistake with the information included on the claim form. The claim is then returned to the practice for correction. A claim denial, on the other hand, is a claim that is received, processed, and then denied.
There are hundreds of technical reasons a claim could be denied, but here are a few of the most common types of denials: Missing or incorrect patient information, like date of birth or date of care. Billing and coding errors, like a procedure for infants being billed for an adult patient.
What Are the Most Common Denial Codes in Medical Billing? CO-4 Missing Medical Modifier. CO-11 Coding Error in Diagnostic Code. CO-15 Missing or Invalid Authorization Number. CO-16 Error or Lack of Information. CO-18 Duplicate Claim or Duplicate Service. CO-22 Coordination of Benefits Error.
CO 129 Payment denied – prior processing information incorrect. Void/replacement error. CO 135 No discharge date permitted for interim claims. CO 151 All dates of service on claim must be within same calendar month, except discharge date can be 1st day of following month.