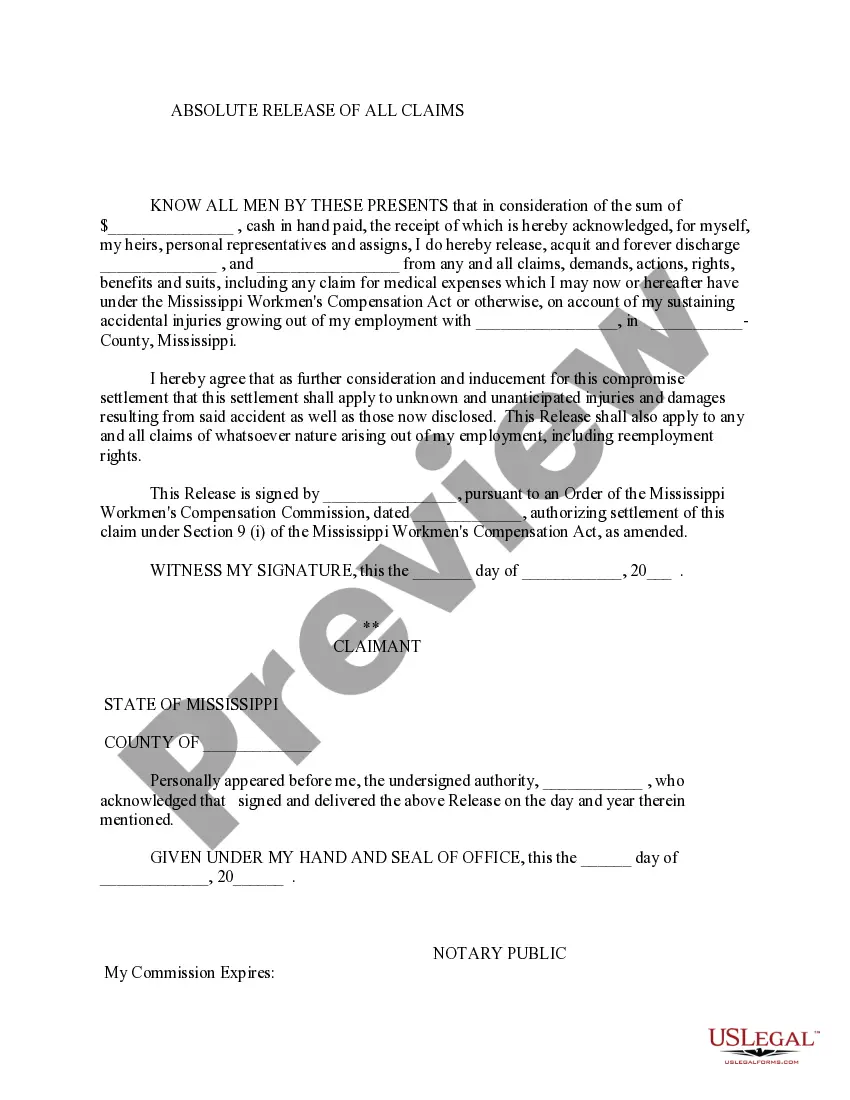
Authorization For Release Of Information
Description
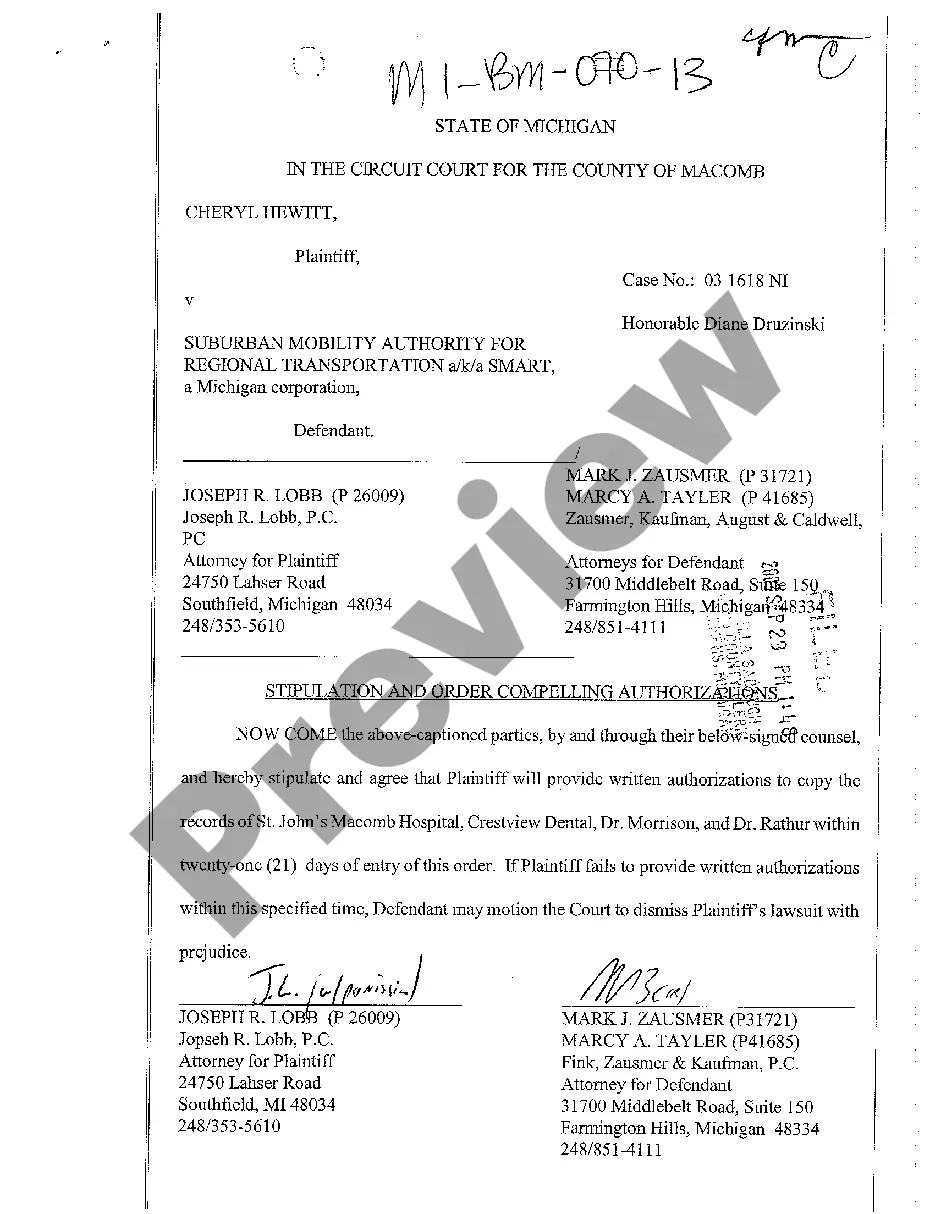
How to fill out Michigan Stipulation And Order Compelling Authorizations?
Maneuvering through the red tape of official documents and formats can be challenging, particularly if one does not engage in that regularly.
Even locating the appropriate format for the Authorization For Release Of Information will be labor-intensive, as it must be accurate and precise to the last detail.
However, you will need to invest significantly less time selecting an appropriate format from a reliable source.
Obtain the correct document in a few straightforward steps: Enter the document's name in the search field. Locate the appropriate Authorization For Release Of Information from the results. Review the description of the example or view its preview. When the format satisfies your requirements, click Buy Now. Continue to select your subscription plan. Utilize your email and create a password to register an account with US Legal Forms. Choose a credit card or PayPal payment method. Save the template document on your device in the format of your preference. US Legal Forms will save you considerable time investigating whether the document you discovered online meets your requirements. Create an account and gain unlimited access to all the documents you need.
- US Legal Forms is a platform that streamlines the process of searching for the correct documents online.
- US Legal Forms is a singular location you require to discover the most current examples of documents, consult their usage, and download these examples for completion.
- This is a compilation with over 85K documents relevant in various employment sectors.
- While looking for an Authorization For Release Of Information, you won't have to doubt its authenticity as all the documents are validated.
- An account with US Legal Forms guarantees you have all the requisite examples at your fingertips.
- Store them in your record or add them to the My documents collection.
- You can retrieve your saved documents from any device by selecting Log In on the library site.
- If you still lack an account, you can always initiate a new search for the format you seek.
Form popularity
FAQ
An authorization is a detailed document that gives covered entities permission to use protected health information for specified purposes, which are generally other than treatment, payment, or health care operations, or to disclose protected health information to a third party specified by the individual.
Release of information (ROI) is the process of providing access to protected health information (PHI) to an individual or entity authorized to receive or review it.
Your authorization allows the Health Plan (your health insurance carrier or HMO) to release your protected health information to a person or organization that you choose.
The core elements of a valid authorization include: A meaningful description of the information to be disclosed. The name of the individual or the name of the person authorized to make the requested disclosure. The name or other identification of the recipient of the information.
You may disclose the PHI as long as you receive a request in writing. The written request must contain: the covered entity's name, the patient's name, the date of the event/time of treatment, and the reason for the request.