Anthem Claim Dispute Form With 2 Points In Riverside
Description
Form popularity
FAQ
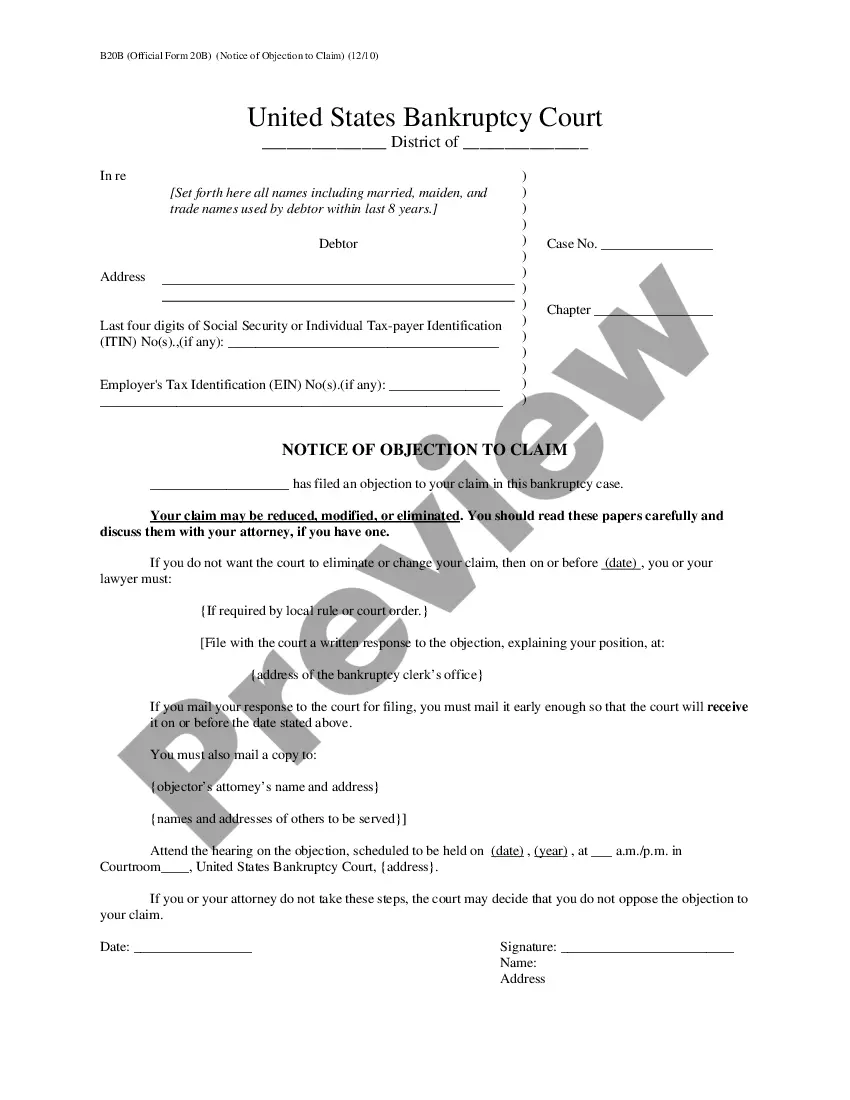
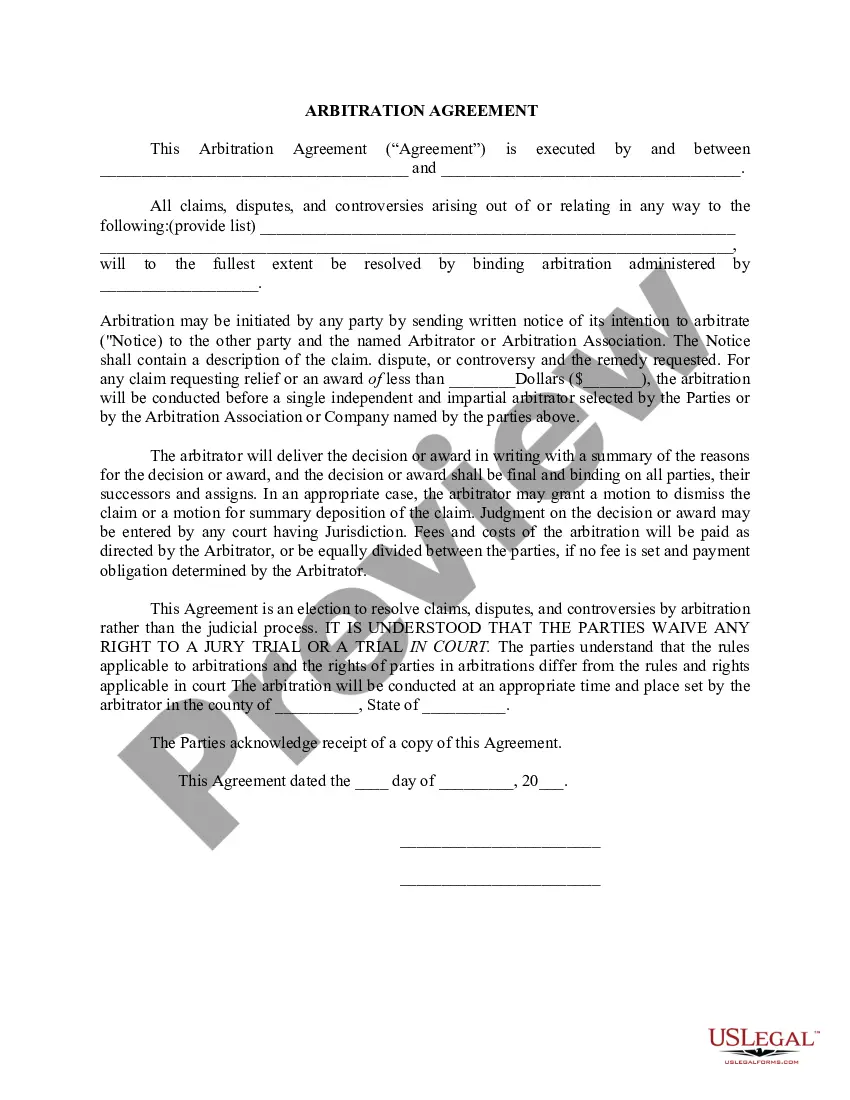
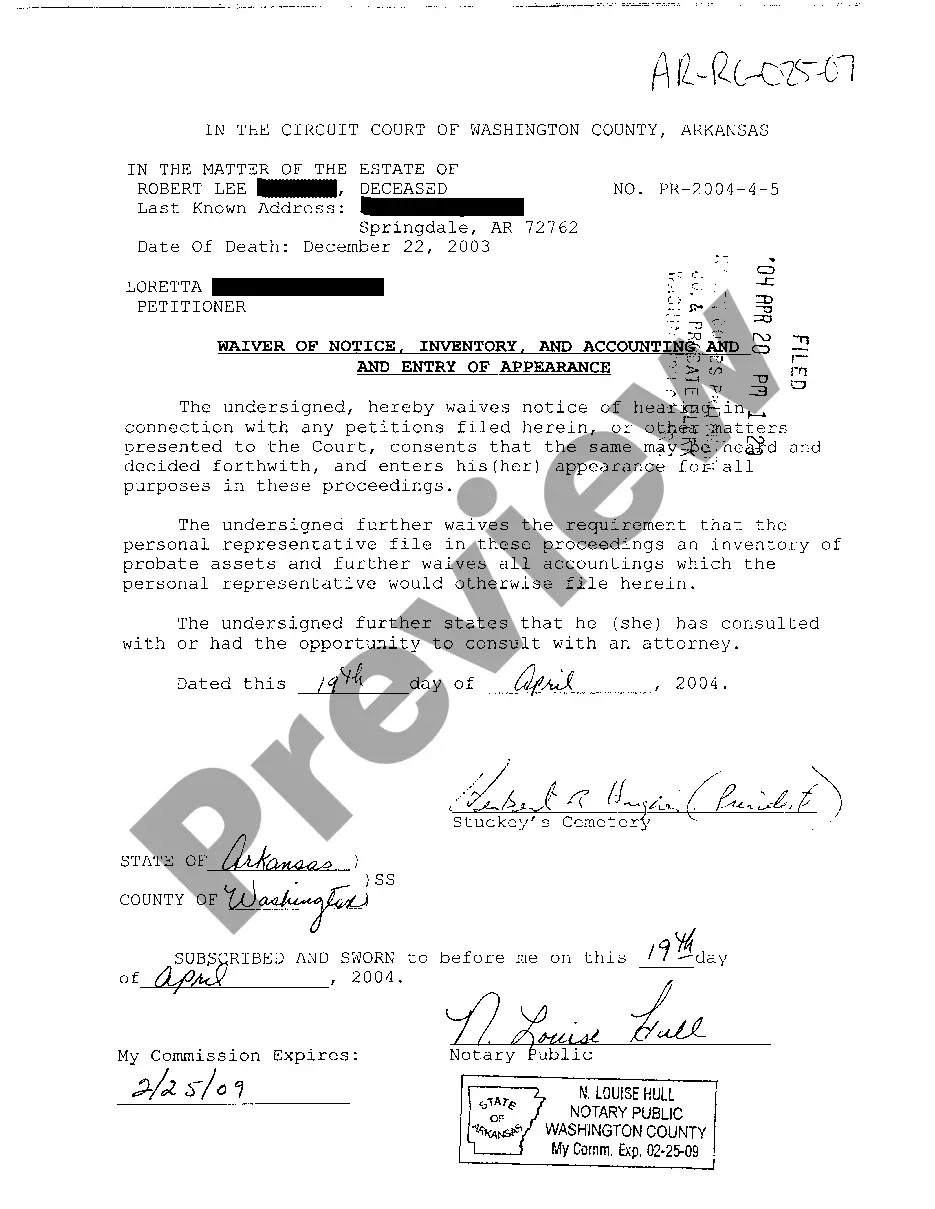
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form. This information is part of the permanent record. Write clearly and legibly.
Customer Care Centers Call 888-831-2246 Option 4 and ask to speak with Dr.
Case Management support is available 24/7 through Anthem Blue Cross Cal MediConnect Plan Customer Care at 1-855-817-5786.
Send this claim to: Blue Shield of California, P.O. Box 272540, Chico, CA, 95927-2540.
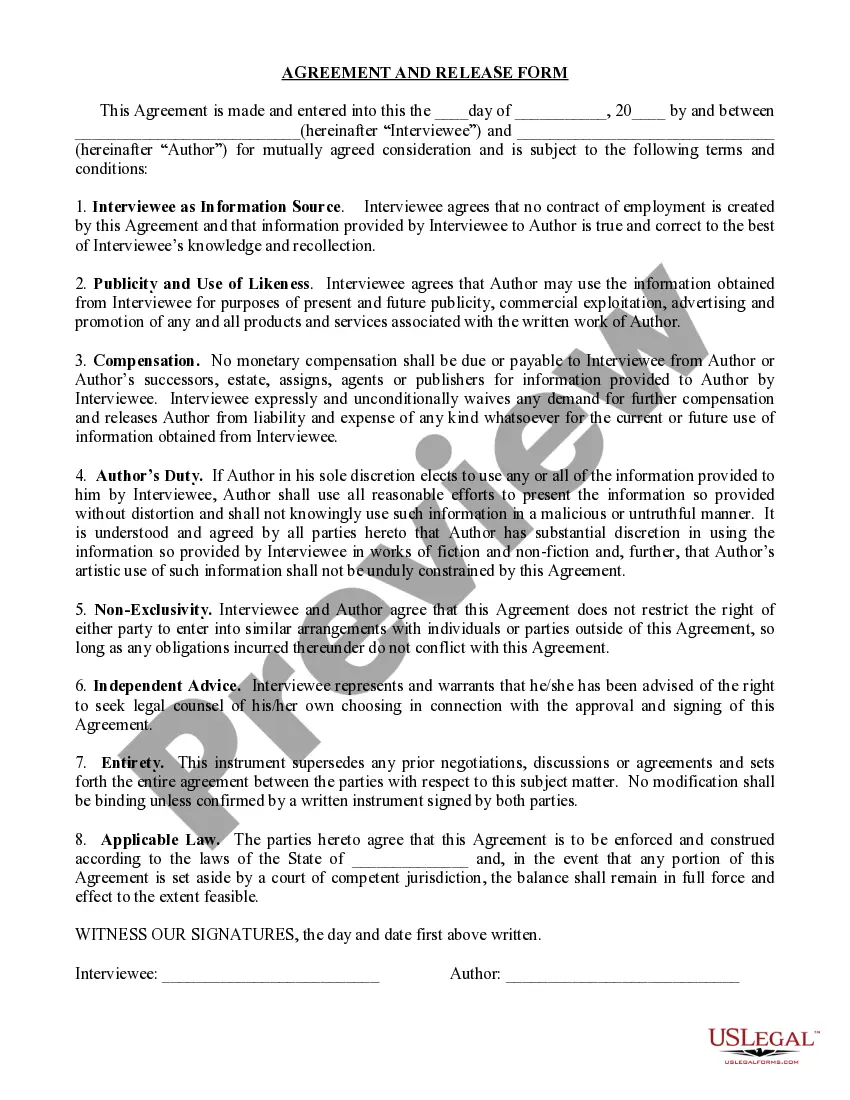
Anthem Blue Cross is the trade name of Blue Cross of California. Anthem Blue Cross and Blue Cross of California Partnership Plan, Inc. are independent licensees of the Blue Cross Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc.
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form.
The appeal must be received by Anthem Blue Cross (Anthem) within 365 days from the date on the notice of the letter advising of the action.
The appeal must be received by Anthem Blue Cross (Anthem) within 365 days from the date on the notice of the letter advising of the action.
With the PPO, you can use any of the BCBS providers in all 50 states. They may not be directly contracted with the BS of CA, but as long as they participate with the BCBS in the state you see a provider in, they will file claims with that plan. Benefits would be covered at the in-network rates given that's the case.
Blue Shield sold Care1st Arizona to WellCare in 2017. Care1st California was renamed Blue Shield of California Promise Health Plan in 2019.