Anthem Claim Dispute Form With 2 Points In Orange
Description
Form popularity
FAQ
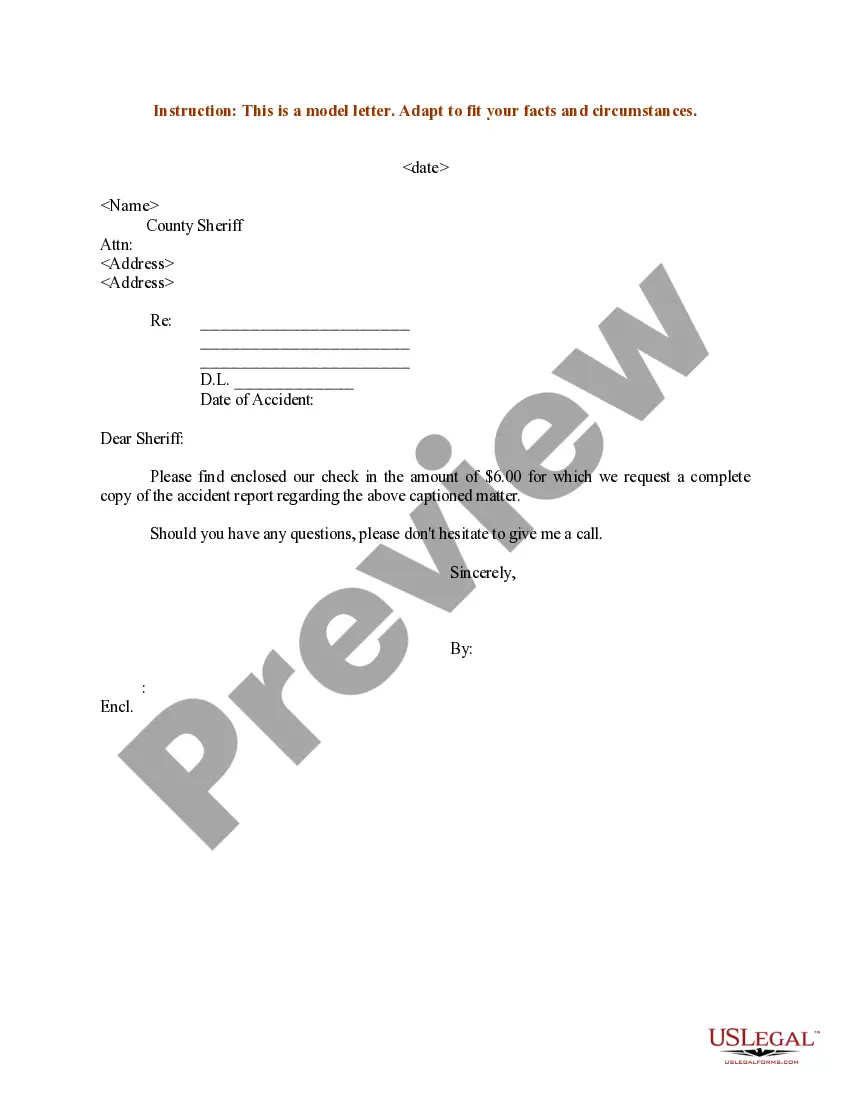
Original (or initial) Medi-Cal claims must be received by the California MMIS FI within six months following the month in which services were rendered. This requirement is referred to as the six-month billing limit.
You need to file your appeal within 60 calendar days from the date on the coverage determination/organization determination notice (denial letter) you received.
The appeal must be received by Anthem Blue Cross (Anthem) within 365 days from the date on the notice of the letter advising of the action.
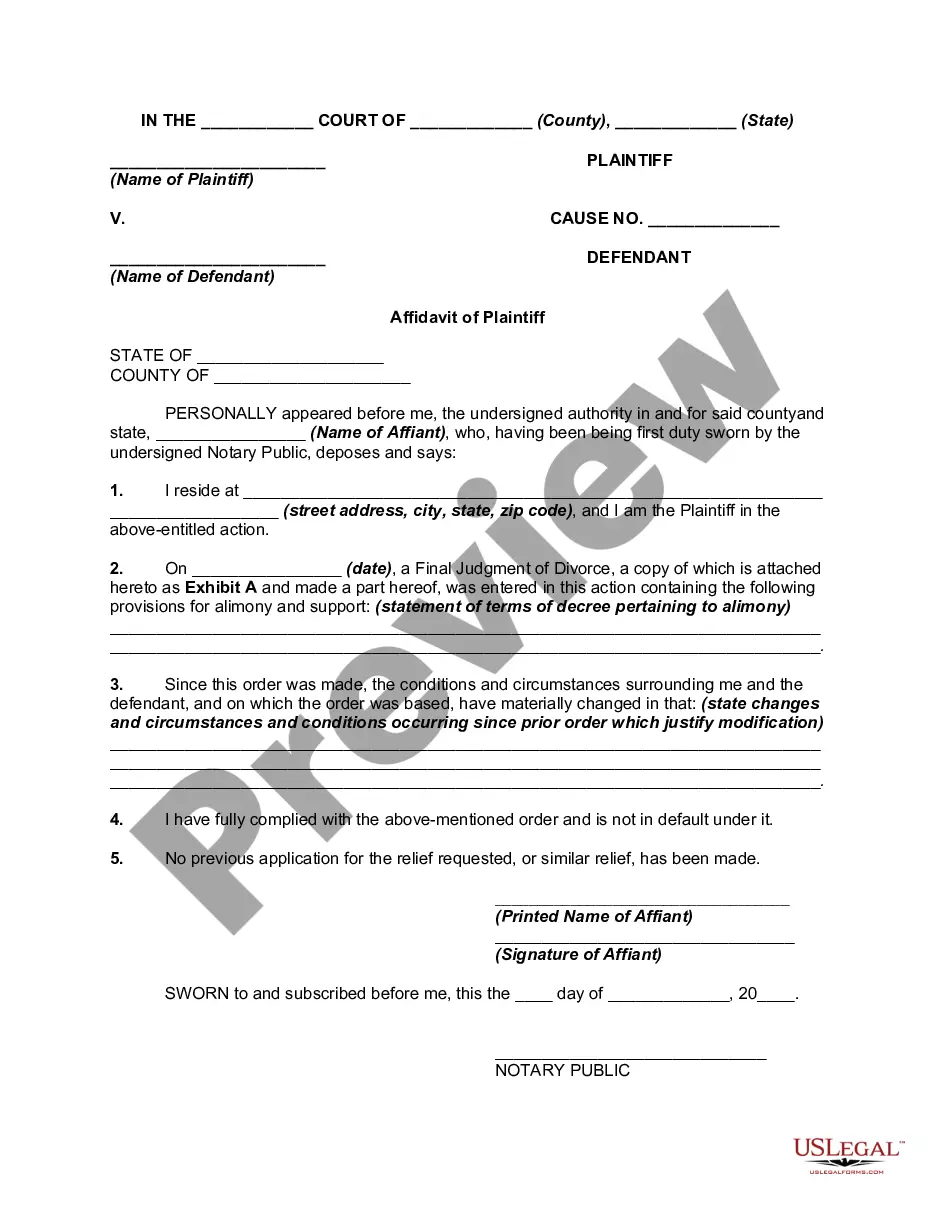
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form. This information is part of the permanent record. Write clearly and legibly.
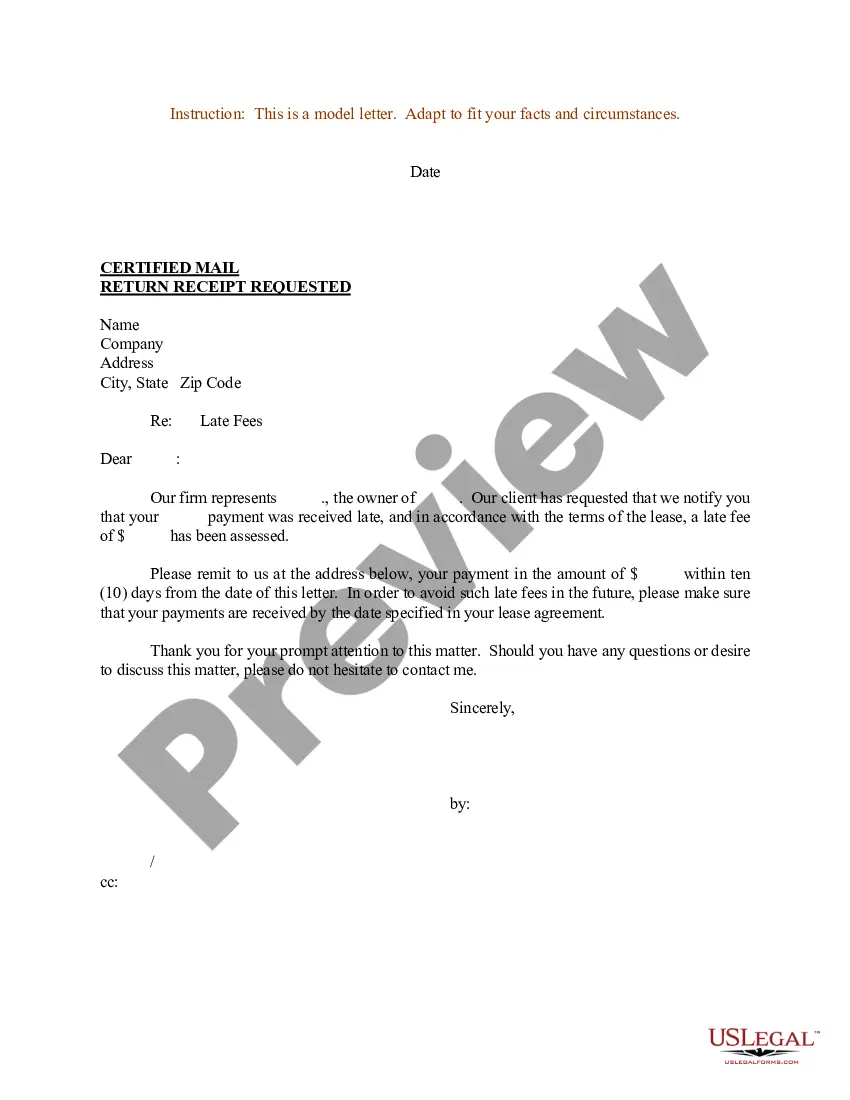
You must do this within 60 calendar days from the date on the Notice of Action sent to you. We will resolve your concerns within 30 days of receiving your complaint. However, if your appeal involves an immediate and serious threat to your health, we will respond to your appeal within 72 hours.
Members have up to 180 calendar days from the date of an incident or dispute, or from the date the member receives a denial letter, to submit a grievance or appeal to Anthem Blue Cross.
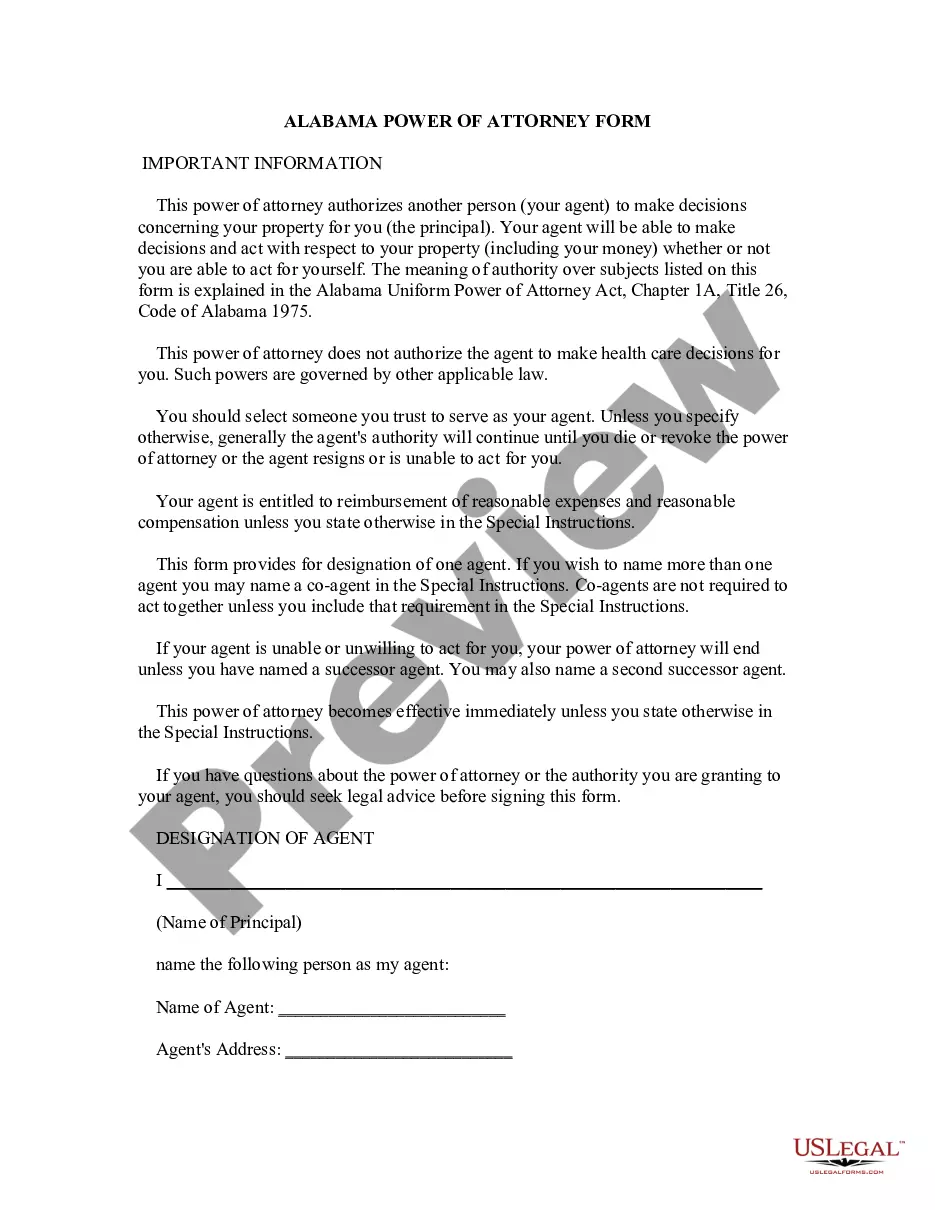
For help, call us at the number listed on your ID card or 1-866-346-7198.
Anthem Blue Cross is the trade name of In California: Blue Cross of California, Anthem Blue Cross Partnership Plan, Anthem BC Health Insurance Company and Anthem Blue Cross Life and Health Insurance Company are independent licensees of the Blue Cross Association.
Customer Care Centers Call 888-831-2246 Option 4 and ask to speak with Dr.