Anthem Claim Dispute Form With 2 Points In Bexar
Description
Form popularity
FAQ
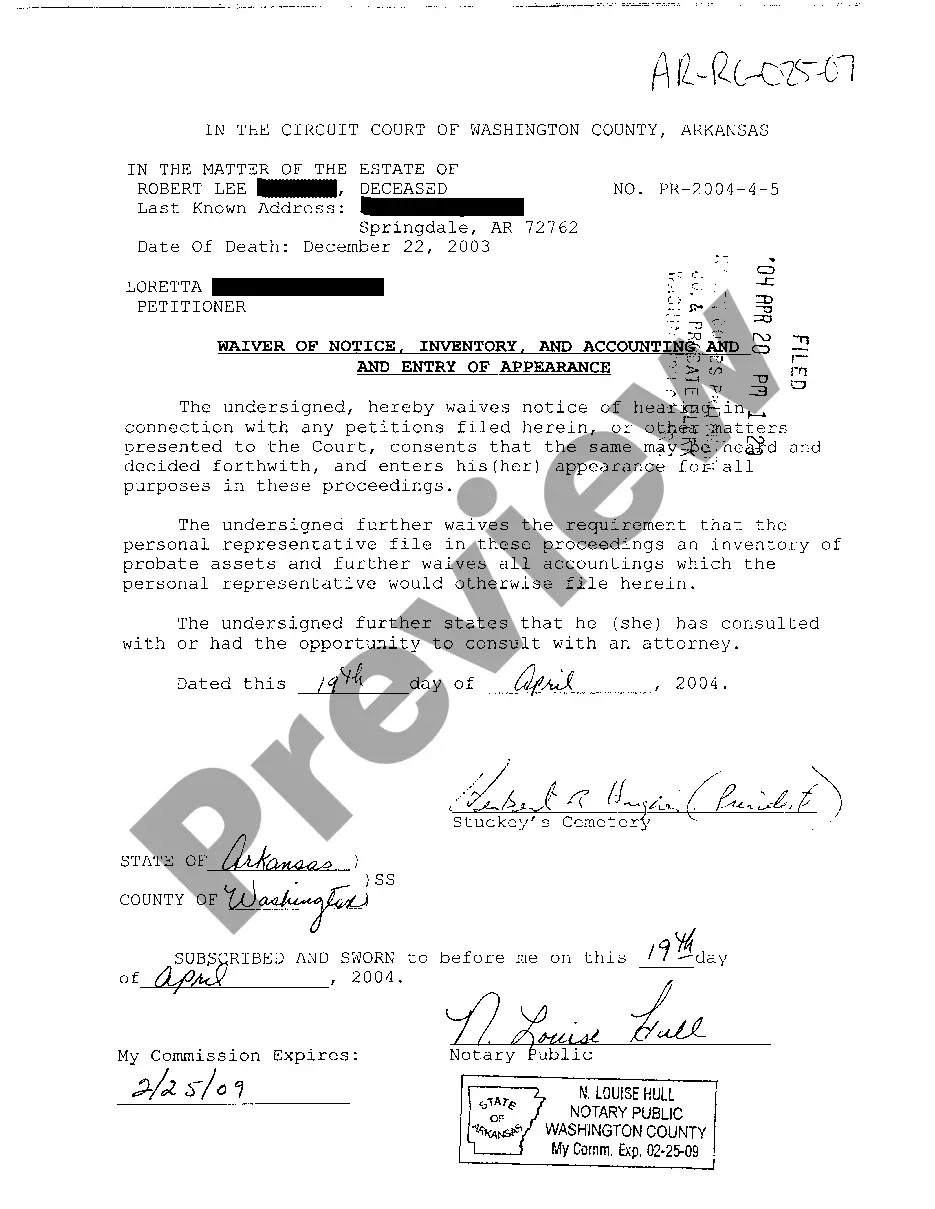
How to Find Timely Filing Limits With Insurance Insurance CompanyTimely Filing Limit (From the date of service) Anthem BCBS Ohio, Kentucky, Indiana, Wisconsin 90 Days Wellmark BCBS Iowa and South Dakota 180 Days BCBS Alabama 2 Years BCBS Arkansas 180 Days28 more rows
Is Anthem the same as Blue Cross Blue Shield? Anthem is part of the Blue Cross Blue Shield group. Blue Cross Blue Shield is made up of independent companies. Anthem is one of these companies.
180-day timely filing limit.
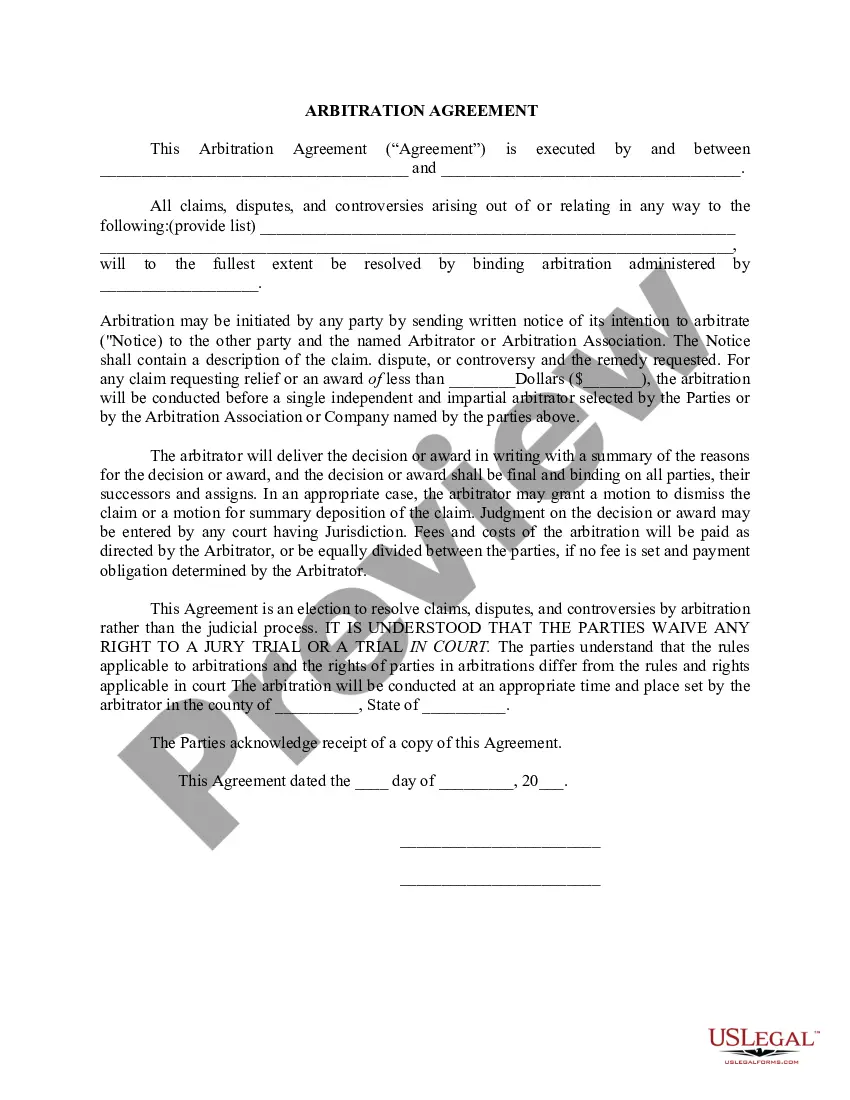
Anthem will consider reimbursement for the initial claim, when received and accepted within timely filing requirements, in compliance with federal, and/or state mandates. Anthem follows the standard of: • 90 days for participating providers and facilities. 15 months for nonparticipating providers and facilities.
Timely filing is when an insurance company put a time limit on claim submission. For example, if a insurance company has a 90-day timely filing limit that means you need to submit a claim within 90 days of the date of service.
-Timely filing is within 180 days of the date of service or per the terms of the provider agreement. Out-of-state and emergency transportation providers have 365 days from the last date of service.
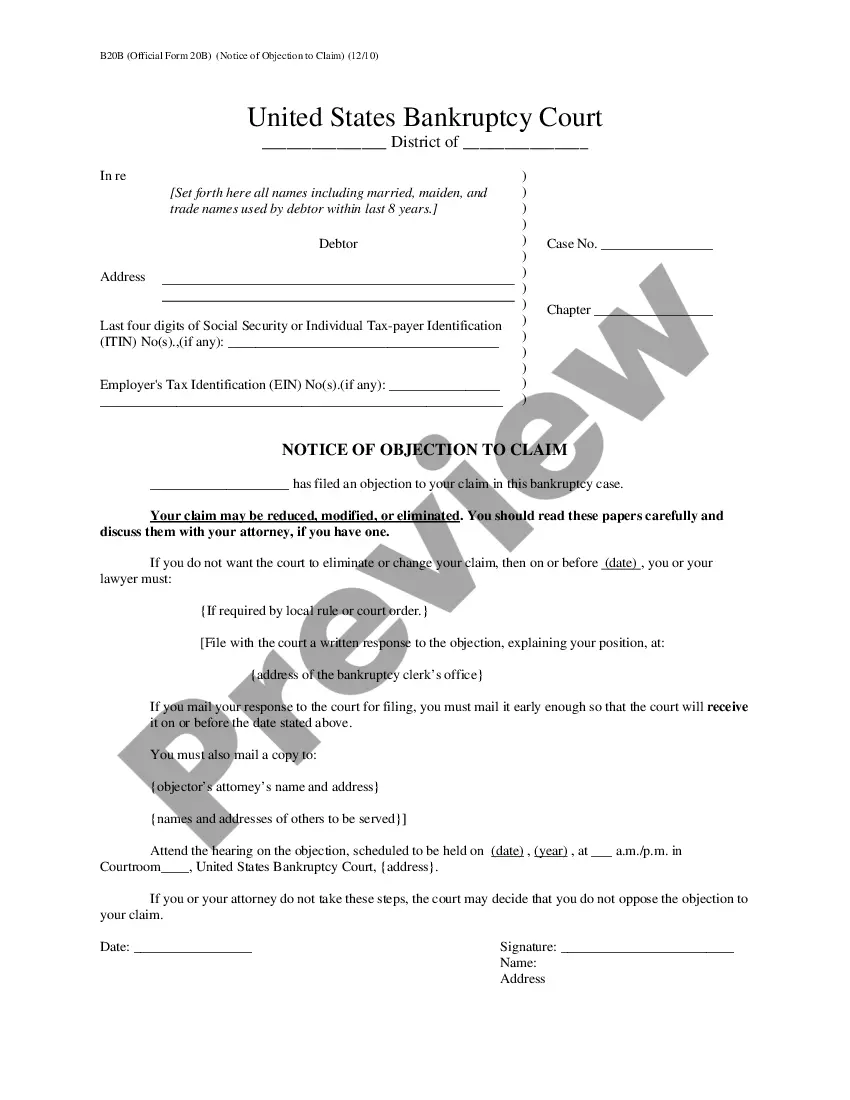
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form. This information is part of the permanent record. Write clearly and legibly.
Your payer name is Anthem BC California and the payer ID is 47198 (If you use a billing company or clearinghouse for your EDI transmissions, please work with them on which payer ID they want you to use.) Questions? We're here to help.
► What is the UnitedHealthcare Payer ID? The Payer ID for UnitedHealthcare commercial plans is 52133.
Our clearinghouse uses payer ID BS001 for Blue Shield, and BC001 for Anthem Blue Cross. In addition to reaching out to the payer directly to confirm where claims need to be submitted, you can also use this Claims routing tool.