Anthem Claim Dispute Form With 2 Points
Description
How to fill out Agreement For Accord And Satisfaction Of A Disputed Claim?
Dealing with legal paperwork and operations might be a time-consuming addition to your entire day. Anthem Claim Dispute Form With 2 Points and forms like it often need you to look for them and navigate the way to complete them effectively. Therefore, regardless if you are taking care of economic, legal, or individual matters, having a comprehensive and practical online catalogue of forms on hand will greatly assist.
US Legal Forms is the number one online platform of legal templates, featuring more than 85,000 state-specific forms and a variety of tools that will help you complete your paperwork easily. Explore the catalogue of pertinent papers available to you with just a single click.
US Legal Forms gives you state- and county-specific forms offered at any moment for downloading. Safeguard your document managing operations having a high quality service that allows you to prepare any form in minutes with no extra or hidden fees. Just log in to your account, find Anthem Claim Dispute Form With 2 Points and download it immediately in the My Forms tab. You may also access formerly saved forms.
Could it be the first time utilizing US Legal Forms? Sign up and set up up an account in a few minutes and you’ll get access to the form catalogue and Anthem Claim Dispute Form With 2 Points. Then, follow the steps listed below to complete your form:
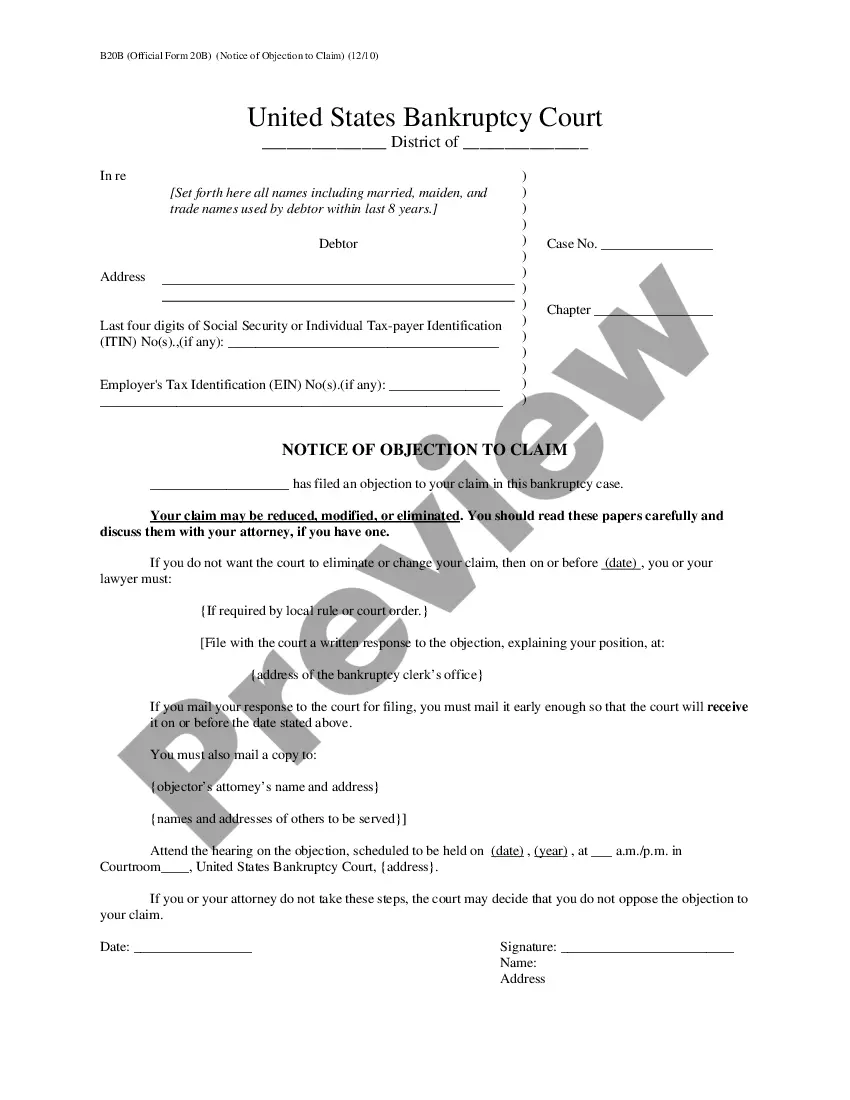
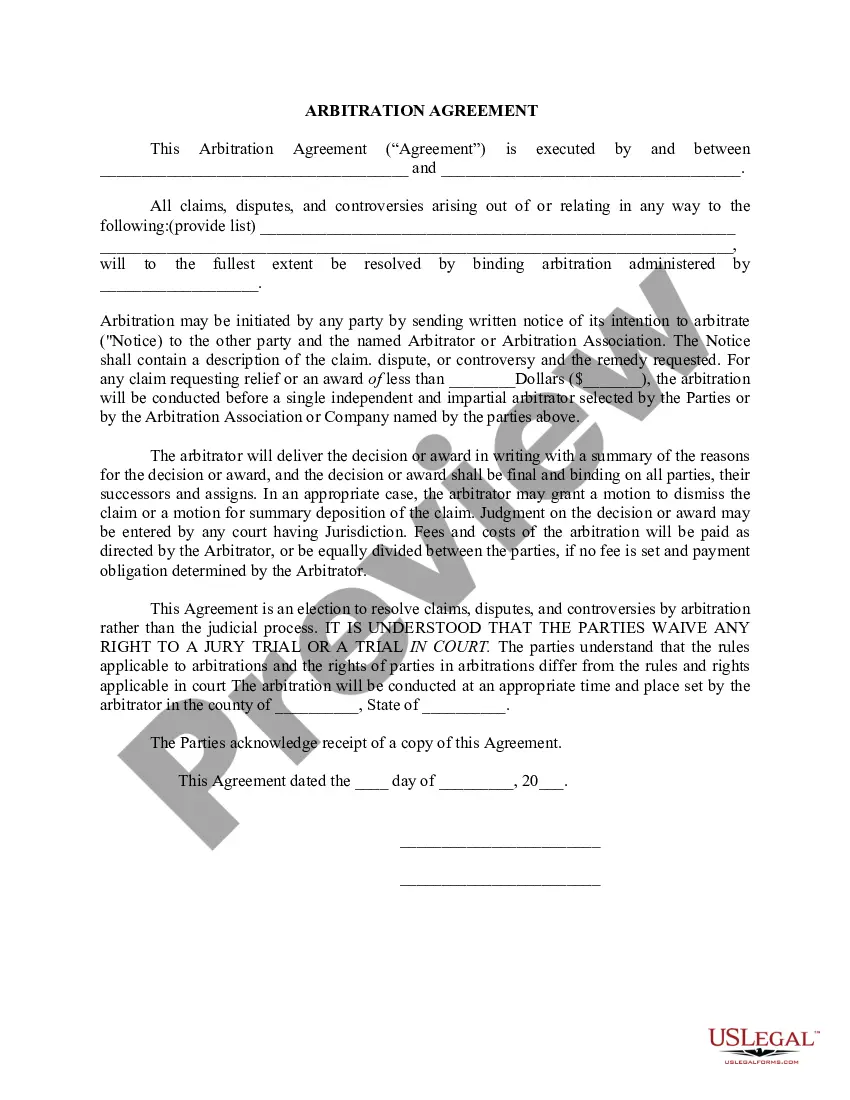
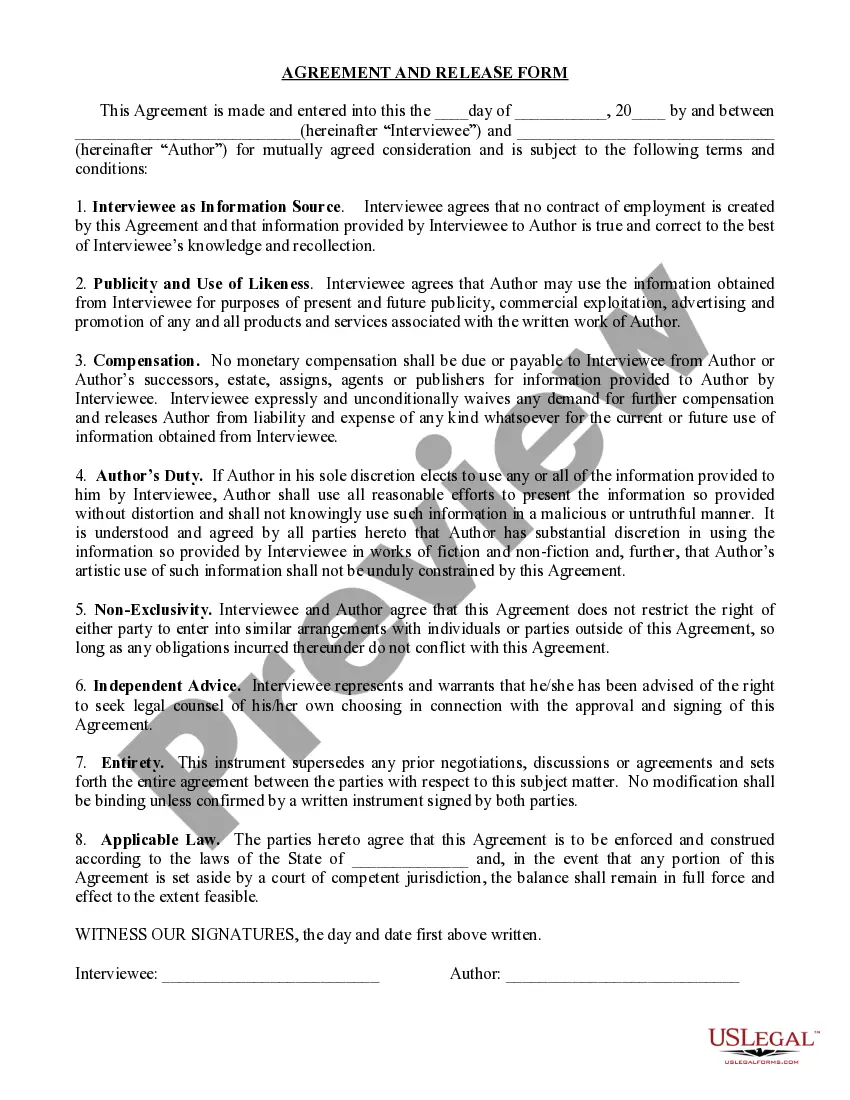
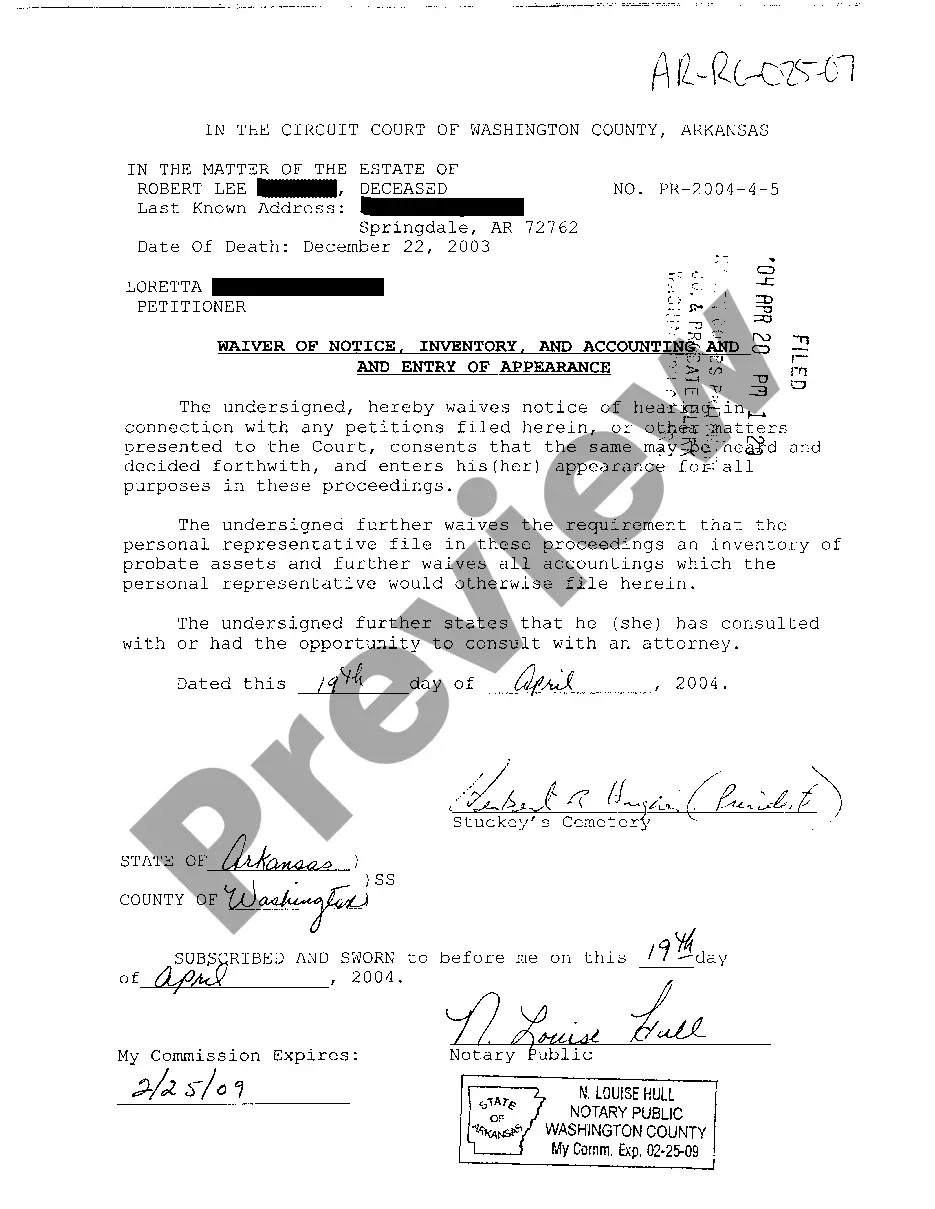
- Be sure you have found the right form by using the Review feature and looking at the form information.
- Choose Buy Now once ready, and select the monthly subscription plan that meets your needs.
- Choose Download then complete, sign, and print the form.
US Legal Forms has twenty five years of experience supporting consumers deal with their legal paperwork. Obtain the form you want right now and streamline any operation without breaking a sweat.
Form popularity
FAQ
Where can an appeal be filed? Mail your written appeal to: Anthem Blue Cross Cal MediConnect Plan. MMP Complaints, Appeals and Grievances. 4361 Irwin Simpson Road. ... Call Member Services at 1-855-817-5785 (TTY: 711) Monday through Friday from 8 a.m. to 8 p.m. This call is free. Fax your written appeal to 1-888-458-1406.
To check claims status or dispute a claim: From the Availity home page, select Claims & Payments from the top navigation. Select Claim Status Inquiry from the drop-down menu. Submit an inquiry and review the Claims Status Detail page. If the claim is denied or final, there will be an option to dispute the claim.
You must file for a medical appeal within 60 calendar days from the date on the Notice of Adverse Benefit Determination letter.
Common Reasons Anthem Gives for Insurance Denials Reasons for Anthem insurance claims denials include: The filing deadline has expired. The insured mad a late payment to COBRA. The medical device or treatment sought is not medically necessary.