Get Nc Bcbs Drug Prior Authorization Request Form 2011-2026
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
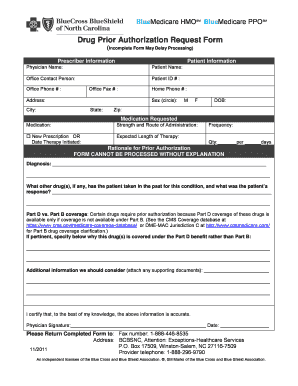
How to fill out the NC BCBS Drug Prior Authorization Request Form online
Filling out the NC BCBS Drug Prior Authorization Request Form online is a crucial step in ensuring your medication request is processed efficiently. This guide will walk you through each section of the form to help you provide the necessary information accurately and thoroughly.
Follow the steps to complete the form online:
- Press the ‘Get Form’ button to obtain the form and open it in the editor.
- Fill in the prescriber information, including the physician's name, office contact person, office phone and fax numbers, and practice address.
- Enter the patient information, which includes the patient’s name, ID number, date of birth, sex (male or female), and complete address including zip code.
- Specify the medication requested by entering the medication name, strength, and route of administration. Indicate whether this is a new prescription and the date therapy was initiated.
- Outline the expected length of therapy, frequency of the medication, and the total quantity prescribed.
- Provide a detailed rationale for the prior authorization request. It’s essential to complete this section as the form cannot be processed without an explanation.
- Include the diagnosis, any previous medications the patient has taken for this condition, and their response to those medications.
- State why the drug is covered under Part D rather than Part B, if applicable, and provide any additional information that may support the request.
- Have the physician sign and date the form, certifying that the information is accurate.
- Submit the completed form via fax to the number provided or through the specified address.
Complete your documents online to ensure a smooth authorization process.
To process pre-authorization, start by consulting with your healthcare provider to determine if prior authorization is necessary for your treatment. They will fill out the appropriate NC BCBS Drug Prior Authorization Request Form, providing the insurance company with the required medical information. Once submitted, your health plan will review the request and inform you of their decision, allowing you to proceed with your treatment if approved.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


