Loading
Get Pharmacy Prior Authorization Form. Request Determination And Authorization For For Members Of
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Pharmacy Prior Authorization Form: Request determination and authorization for members online
Filling out the Pharmacy Prior Authorization Form is an essential step for individuals seeking medication approvals. This guide provides a clear, step-by-step approach to assist you in completing this form accurately and efficiently.
Follow the steps to fill out the Pharmacy Prior Authorization Form
- Press the ‘Get Form’ button to access the Pharmacy Prior Authorization Form and open it for editing.
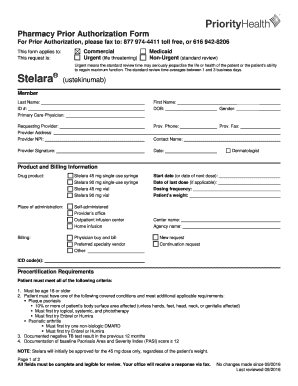
- Begin by filling in the member's last name, first name, and date of birth (DOB) in the designated fields. Also, include the member's ID number and gender.
- Next, provide details about the requesting provider, including their name, address, National Provider Identifier (NPI), phone number, and fax number. Ensure that all information is accurate for correspondence.
- In the product and billing information section, select the appropriate drug product from the listed options, such as 45 mg single-use syringe or 90 mg vial. Fill in the start date or date of the next dose, the date of the last dose (if applicable), and the dosing frequency.
- Indicate the patient’s weight and the place of administration (e.g., self-administered, provider’s office). If applicable, include the name of the center and billing method.
- Choose whether this is a new request or a continuation request, and provide the appropriate ICD code(s) that best represent the patient’s condition.
- Complete the precertification requirements by ensuring the patient meets all specified criteria. Document the date and result of the patient’s most recent tuberculosis (TB) test and baseline Psoriasis Area and Severity Index (PASI) score.
- If applicable, provide rationale for dose increases according to the specified requirements, including response to past treatments and current PASI scores.
- Review the form to ensure all fields are complete and legible. Finally, ensure to save changes to the document, then download, print, or share the form as required.
Complete your Pharmacy Prior Authorization Form online today for efficient processing.
A decision by your health insurer or plan that a health care service, treatment plan, prescription drug or durable medical equipment is medically necessary. Sometimes called prior authorization, prior approval or precertification.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


