Loading
Get Preauthorization Request Form - Univera Healthcare
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Preauthorization Request Form - Univera Healthcare online
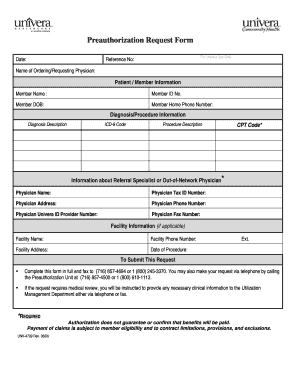
Filling out the Preauthorization Request Form for Univera Healthcare is an essential step in the healthcare process. This guide will assist you in completing the form online, ensuring that all necessary information is accurately provided.
Follow the steps to fill out the form effectively.
- Click ‘Get Form’ button to obtain the form and open it in the editor.
- Fill out the section titled ‘For Univera Use Only’ by leaving the reference number blank, as this will be assigned by Univera after submission.
- Provide the name of the ordering or requesting physician. This is crucial for identifying who is making the request.
- In the ‘Patient / Member Information’ section, enter the member's name, member ID number, and their date of birth. Additionally, include the member's home phone number for contact purposes.
- Next, describe the diagnosis and include the ICD-9 code, which identifies the diagnosis. Then, detail the procedure description and the corresponding CPT code, if applicable.
- If applicable, fill in the information about the referral specialist or out-of-network physician. Enter their name, tax ID number, address, phone number, Univera ID provider number, and fax number.
- Complete the facility information if this procedure will occur in a facility. This includes the facility name, phone number, address, and the date of the procedure.
- Review all entries for accuracy and completeness to ensure that the submission is processed smoothly.
- To submit this request, you can fax the completed form to (716) 857-4694 or 1 (800) 245-3370. Alternatively, you may contact the Preauthorization Unit at (716) 857-4500 or 1 (800) 610-1113 for further assistance.
- After submission, it is advisable to save any changes you made, download a copy for your records, print the document, or share it as needed.
Complete your Preauthorization Request Form online today to ensure timely processing of your request.
A prior authorization decision may take up to 24 to 72 hours. How do I check the status of a prior authorization request? You can call the Member Services phone number on your member ID card from 7 a.m. to 7 p.m. Pacific time, Monday through Friday, or you can call your doctor's office.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


