Loading
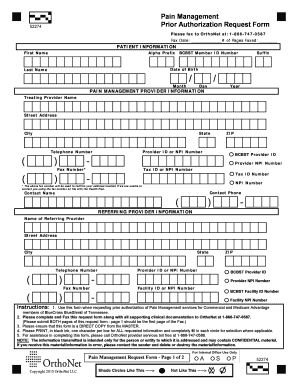
Get Bcbstn - Pm Req Frm-fnl--2016x 52274 - Activated Traditional
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the BCBSTN - PM Req Frm-FNL--2016X 52274 - Activated Traditional online
This guide provides clear, step-by-step instructions for completing the BCBSTN - PM Req Frm-FNL--2016X 52274 - Activated Traditional form online. Ensuring accuracy in your submission will help expedite your request for prior authorization of pain management services.
Follow the steps to accurately complete the prior authorization request form.
- Click the ‘Get Form’ button to obtain the form and access it in your chosen online editor.
- Begin by filling out the patient information section. Input the patient's first name, last name, date of birth, BCBST member ID number, and any relevant prefixes or suffixes as needed.
- Next, move to the pain management provider information section. Fill in the treating provider's name, address, state, city, telephone number, provider ID or NPI number, and tax identification number.
- Proceed to the referring provider information section. Here, you will input the name, address, city, state, telephone number, and provider identification numbers of the referring provider.
- In the request information section, begin by entering the primary diagnosis code using ICD-10 format. Then select the appropriate spinal region(s) that apply.
- Specify the requested procedures by selecting from the various listed options, such as spinal cord stimulators or pain pumps.
- Provide exact details on the injection sites, including whether they will be left, right, or bilateral, and the site of injection. This information is vital for processing the request.
- Indicate how many injections have occurred in the past 12 months and provide the date of the last injection.
- Complete the CPT codes, place of service, and anticipated date of service sections as required.
- After filling out all sections accurately, review your entries for completeness before saving changes or sharing the form as necessary.
Start filling out your pain management prior authorization request form online today to ensure timely processing.
Prior authorization (PA) may be required via BCBSTX's medical management, eviCore® healthcare, Carelon Medical Benefits Management effective March 1, 2023 (formerly AIM) or Magellan Healthcare®. You can review how to submit PA or Notification requests and view PA statistical data here.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


