Loading
Get Osteoporosis Precertification Request Form - Aetna
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Osteoporosis Precertification Request Form - Aetna online
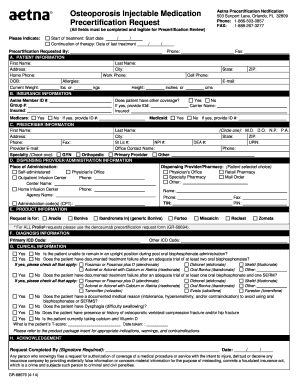
Filling out the Osteoporosis Precertification Request Form is an essential step in obtaining necessary medication for osteoporosis treatment. This guide will provide clear instructions to help you complete the form correctly and efficiently online.
Follow the steps to fill out the form accurately.
- Click ‘Get Form’ button to obtain the form and open it in the editor.
- Begin by entering the patient's information in section A. Fill out all required fields, including first name, last name, address, phone numbers, date of birth, allergies, height, and any relevant member ID numbers.
- In section B, provide the insurance information, including Aetna member ID number, group number, and any other coverage details, if applicable.
- Proceed to section C to enter the prescriber information. Fill out the prescriber's first and last name, address, contact information, and professional details, including their medical credential.
- In section D, indicate the dispensing provider or pharmacy choice. Choose from options like physician's office, retail pharmacy, specialty pharmacy, or mail order and provide their contact information.
- Move to section E, where you will select the requested medication from the product list, ensuring to specify any administration codes if necessary.
- Fill out section F by providing the primary and any additional ICD codes related to the patient's diagnosis.
- In section G, answer the clinical questions about the patient's condition and treatment. Be sure to provide detailed information regarding treatment failures and current medications.
- Finally, review the form for accuracy. Once everything is complete, you can save changes, download, print, or share the form as necessary.
Complete the Osteoporosis Precertification Request Form online to ensure timely processing of your precertification request.
Retrospective review is available when: Precertification/notification requirements were met at the time the service was provided, but the dates of service do not match the submitted claim. Aetna converts from secondary payer to primary payer at the time of inpatient claims adjudication.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


