Loading
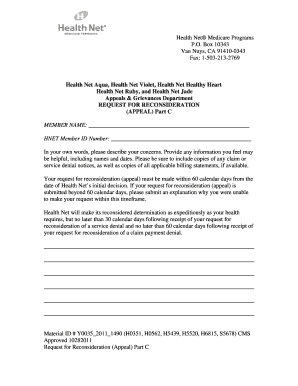
Get Health Net Appeal Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Health Net appeal form online
Filling out the Health Net appeal form online is a straightforward process that allows users to formally request a reconsideration of decisions related to their Medicare coverage. This guide will provide clear instructions to ensure that you successfully complete the form and submit it appropriately.
Follow the steps to complete your request for reconsideration.
- Click ‘Get Form’ button to obtain the form and open it in the editor.
- Begin by entering your full name in the 'Member Name' field. Ensure that the spelling is correct as it will be used to identify your account.
- In the 'HNET Member ID Number' field, provide your unique member identification number. This number is essential for processing your appeal.
- Next, in the designated section, clearly describe your concerns in your own words. Be detailed and include any relevant information, such as names, dates, and specifics about the decision you are appealing.
- If applicable, attach copies of any claim or service denial notices. Also, include all relevant billing statements that support your appeal.
- Remember that your request for reconsideration must be submitted within 60 calendar days from the date of Health Net’s initial decision. If you are submitting after this period, explain why you were unable to do so in a timely manner.
- After you have filled out all necessary fields and sections, review the form for accuracy and completeness.
- Finally, save your changes. Then, download, print, or share the form as needed. Ensure that it is sent to the appropriate address provided on the form.
Complete your Health Net appeal form online today and ensure your voice is heard.
Related links form
Timely Filing of Claims When Health Net is the secondary payer, we will process claims received within 180 days after the later of the date of service and the date of the physician's receipt of an Explanation of Benefits (EOB) from the primary payer.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


