Loading
Get Provider Appeal Request Form - Wellcare
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Provider Appeal Request Form - WellCare online
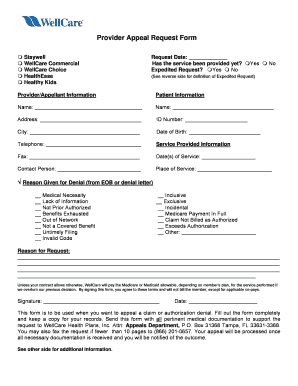
Filling out the Provider Appeal Request Form for WellCare is an important step in addressing claim or authorization denials. This guide provides clear instructions to navigate the process effectively online.
Follow the steps to complete your Provider Appeal Request Form.
- Click ‘Get Form’ button to retrieve the Provider Appeal Request Form and open it in your chosen editor.
- Enter the request date in the designated field provided on the form.
- Indicate whether the service has been provided by selecting 'Yes' or 'No'.
- If applicable, mark if this is an expedited request by selecting 'Yes' or 'No'. Refer to the reverse side for the definition of an expedited request.
- Fill out the 'Provider/Appellant Information' section with your details, including name, address, and contact information.
- Provide the patient's information by entering their name, address, ID number, city, date of birth, and telephone number.
- In the 'Service Provided Information' section, detail the date(s) of service and the place of service.
- Select the reason for denial by checking the appropriate boxes provided that correspond to the explanation found in the Explanation of Benefits (EOB) or denial letter.
- In the 'Reason for Request' section, clearly explain the rationale for your appeal. Include any important details that support your case.
- Sign and date the form to affirm your agreement to the terms outlined.
- Once you have filled out all sections completely, save your changes, and choose to download, print, or share the completed form as necessary.
Complete the Provider Appeal Request Form online today to address your claims effectively.
The Claim Payment Dispute Process is designed to address claim denials for issues related to untimely filing, unlisted procedure codes, non-covered codes etc. Claim payment disputes must be submitted in writing to Wellcare within 90 calendar days of the date on the EOP.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


