Loading
Get 8669591537
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the 8669591537 online
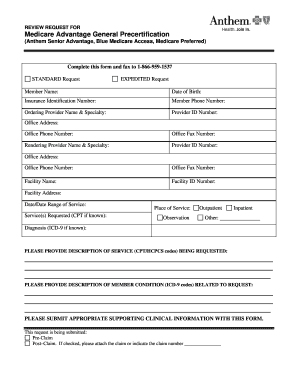
Filling out the 8669591537 form effectively is crucial for requesting Medicare Advantage precertification. This guide provides clear instructions on how to complete each section of the form to ensure your submission is accurate and complete.
Follow the steps to effectively complete the 8669591537 form.
- Click the ‘Get Form’ button to obtain the form and open it in the editor for online completion.
- Begin by entering the member's name in the designated field. This should be the full legal name of the individual requesting service.
- Input the member's date of birth in the format requested (MM/DD/YYYY). This helps in verifying the identity of the member.
- Provide the insurance identification number associated with the member. This number is typically found on the member's insurance card.
- Enter the member's phone number for contact purposes, ensuring it is correct to facilitate potential follow-ups.
- Fill in the ordering provider's name and specialty as it appears in their records. Include the provider's ID number.
- Specify the office address, phone number, and fax number of the ordering provider to ensure correspondence is directed properly.
- Complete the rendering provider's information in the same manner as the ordering provider, including their specialty and ID number.
- List the facility name, facility ID number, and the facility address where the service is being requested.
- Indicate the date or date range of the service being requested. This helps in scheduling and validating the need for precertification.
- Provide a clear description of the services requested, including any known CPT codes, which are essential for processing the request.
- Select the place of service (i.e., observation, outpatient, inpatient, or other) by marking the appropriate option.
- Document the diagnosis related to the request, including ICD-9 codes if known, as this supports the medical necessity aspect of the request.
- Supply a detailed description of the service being requested, including relevant CPT/HCPCS codes.
- Provide a description of the member's condition related to the request, again including ICD-9 codes where applicable.
- Attach any appropriate supporting clinical information with the form, as this is essential for a thorough review of the request.
- Indicate whether the request is a pre-claim or post-claim. If post-claim is selected, remember to attach the relevant claim or provide the claim number.
- Complete the attestation by having the provider or their representative print their name, title, and date of completion within the designated fields.
- Once all fields are accurately filled out, review the information for completeness and correctness. After verification, save any changes, download a copy, or print and share the form as needed.
Complete your documents online to ensure a smooth submission process.
Pre-auth status refers to whether a health service or procedure has received prior authorization from an insurance company. This confirmation is necessary before proceeding to ensure coverage. You can learn more about your pre-auth status by using the number 8669591537 for fast assistance. Understanding this process can help clarify your coverage and avoid unexpected costs.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


