Get Medco Prior Auth Form 2020-2025
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Medco Prior Auth Form online
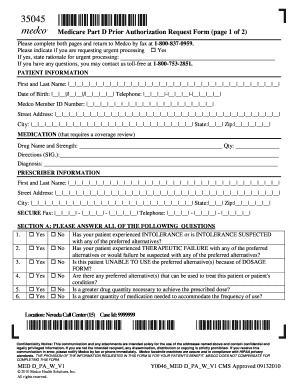
The Medco Prior Authorization Form is essential for obtaining medication coverage approval under Medicare Part D. This guide will provide you with clear and comprehensive steps to accurately complete this form online, ensuring that all necessary information is included for a successful submission.
Follow the steps to effectively complete the Medco Prior Auth Form online.
- Click ‘Get Form’ button to obtain the form and open it in the editor.
- Begin by entering the patient information in the designated fields. Include the patient's full name, date of birth, telephone number, and Medco member ID number.
- Provide the patient's street address, city, state, and zip code. Ensure all required information is filled in accurately.
- In the medication section, specify the drug name and its strength required for coverage review. Indicate the quantity required and provide dosing instructions along with the diagnosis.
- Under prescriber information, enter the prescriber’s full name, street address, city, state, and zip code. Include the prescriber’s secure fax number and telephone number.
- Answer all questions in Section A truthfully by selecting 'Yes' or 'No' regarding the patient’s experience with alternatives and the necessity of the prescribed medication.
- If applicable, complete Section B questions regarding the prescriber’s participating status with Medicare and the patient's enrollment in Part B coverage.
- If the patient is using immunosuppressant medications, answer the questions in Section C. If chemotherapy agents are involved, complete Section D questionnaire.
- Provide any additional rationale in Section E if needed to support the request.
- Finally, have the prescriber sign the form and submit it by faxing the completed document to 1-800-837-0959. You may save changes, download, print, or share the form as necessary.
Start filling out the Medco Prior Auth Form online today to ensure timely medication coverage!
Yes, Aetna often requires prior authorization for certain treatments and medications. This requirement helps ensure that the proposed treatments are medically necessary and covered under the policy. You may need to complete the Medco Prior Auth Form as part of this process. Checking specific Aetna guidelines can help clarify when prior authorization is needed.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


