Loading
Get Qualcare Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Qualcare Prior Authorization Form online
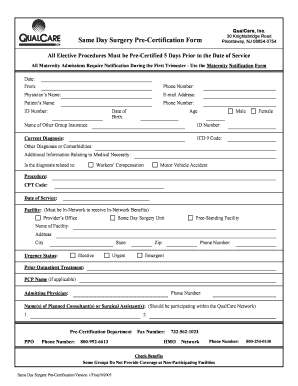
Filling out the Qualcare Prior Authorization Form accurately is essential for ensuring timely medical service approvals. This guide provides a clear and supportive approach to completing the form online, making the process as straightforward as possible.
Follow the steps to successfully complete the form
- Press the ‘Get Form’ button to access the Qualcare Prior Authorization Form and open it in the document editor.
- Begin by entering the date and the name of the person completing the form in the designated fields.
- Provide your phone number and the physician’s name, followed by their email address.
- Fill in the patient’s information, including their name, phone number, ID number, date of birth, and age. Indicate the sex of the patient by selecting either male or female.
- If applicable, include the name and ID number of any other group insurance the patient may have.
- Specify the current diagnosis and the corresponding ICD 9 code. If there are additional diagnoses or comorbidities, provide that information in the designated area.
- Indicate whether the diagnosis relates to workers’ compensation or a motor vehicle accident, if applicable.
- Describe the procedure by entering the CPT code and the date of service in the appropriate fields.
- Select the facility type, ensuring it is in-network to receive benefits, and enter the facility's name and address.
- Choose the urgency status by indicating whether the procedure is elective, urgent, or emergent.
- If there was prior outpatient treatment, include the relevant information of the primary care physician, including their name and phone number.
- Enter the admitting physician’s name and the names of any planned consultants or surgical assistants participating within the Qualcare network.
- Provide the contact information for the pre-certification department, including the PPO and HMO phone numbers.
- Review the entire form for accuracy, make any necessary corrections, and then proceed to save the changes, download, print, or share the completed form as needed.
Complete your Qualcare Prior Authorization Form online today for a smooth pre-certification process.
A prior authorization for Ozempic means your healthcare provider must obtain approval from your insurance before you receive the medication. The Qualcare Prior Authorization Form typically includes information about your medical condition and treatment history. This process ensures that Ozempic is necessary and appropriate for your care.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


