Get Sample Written History And Physical Examination
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Sample Written History And Physical Examination online
Filling out the Sample Written History And Physical Examination is an essential step in documenting a patient's medical history and current condition. This guide provides clear, step-by-step instructions to help ensure that all necessary information is captured accurately and efficiently.
Follow the steps to complete the form effectively.
- Press the ‘Get Form’ button to access the Sample Written History And Physical Examination and open it in your preferred editor.
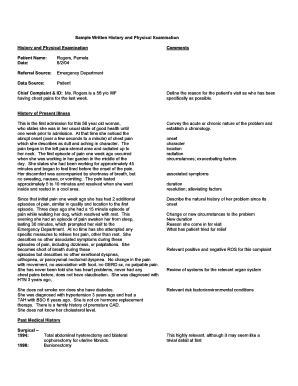
- Begin by entering the patient's name and the date of examination at the top of the form. Ensure that the patient's information is accurate and up-to-date.
- Next, fill in the referral source. Specify where the patient was referred from, such as the emergency department, to provide context for the examination.
- In the section for chief complaint and identification, clearly define the primary issue the patient is experiencing. Be as specific as possible, noting details such as onset, duration, and severity of symptoms.
- Proceed to the history of present illness section. Describe the patient's current health condition, including the chronology of symptoms and any factors that may exacerbate them.
- List relevant past medical history, including any surgeries, diagnosed conditions, allergies, and medications. This information is crucial for understanding the patient's background.
- Complete the family history section, detailing any significant health issues among close relatives. This can provide insight into potential hereditary conditions.
- Document any relevant review of systems, noting both positive and negative findings briefly. This helps to identify any additional concerns not initially mentioned.
- Fill out the physical examination section, capturing vital signs and observations of each body system. Be thorough in noting any abnormalities that may impact the patient's care.
- For the assessment and differential diagnosis, summarize the doctor’s clinical findings, potential diagnoses, and any necessary follow-up actions.
- Finally, detail the plan for the patient's care, including medications, tests, and lifestyle recommendations. This comprehensive overview will assist in guiding future treatment.
- Once all sections are completed, review the document for accuracy. Users can then save changes, download, print, or share the completed form as necessary.
Start filling out your Sample Written History And Physical Examination online today for efficient patient documentation.
HPI format, or History of Present Illness, typically follows a structured approach to documenting a patient's current health issues. Start with a brief description of the symptoms, followed by details such as when they began, any exacerbating factors, and alleviating measures. Ensure to maintain clarity and conciseness to create an effective Sample Written History And Physical Examination that supports your clinical decision-making.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


