Get Molina Healthcare Provider Dispute Resolution Request 2010-2025
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Molina Healthcare Provider Dispute Resolution Request online
Filling out the Molina Healthcare Provider Dispute Resolution Request is an important step in resolving billing disputes. This guide provides a clear and supportive walkthrough on how to complete the form online, ensuring you provide all necessary information for a successful resolution.
Follow the steps to complete the Molina Healthcare Provider Dispute Resolution Request online.
- Press the ‘Get Form’ button to access the Provider Dispute Resolution Request and open it in your preferred editor.
- Fill in the required fields marked with an asterisk (*), starting with the provider name and tax ID or Medicare ID number, ensuring accurate information.
- Enter the provider address and select the provider type from the available options, including MD, mental health, home health, and more.
- In the claim information section, indicate whether you are submitting a single claim or multiple claims. If multiple claims, complete the attached spreadsheet with the specified number of claims.
- Provide the patient’s name and health plan ID number, along with their date of birth and account number.
- Include the service dates (from/to) as it is required for claims and overpayment disputes.
- Fill out the original claim ID number and original claim amount billed.
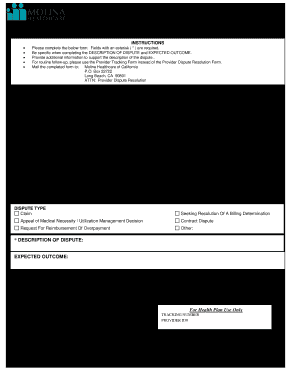
- In the dispute type section, check the appropriate box that reflects your reason for the dispute, such as claim resolution, appeal of medical necessity, or contract dispute.
- Clearly describe the dispute and expected outcome in the relevant fields, being specific and providing any additional supporting information if necessary.
- Enter contact information including name, title, phone number, and add your signature and date at the bottom of the form.
- If additional information is needed, check the box indicating attachments and remember not to staple documents.
- Once all information is filled in, save changes, and download or print the form for your records before mailing it to the provided address.
Complete your dispute resolution request online today for a smooth and efficient process.
The four types of dispute resolution include negotiation, mediation, arbitration, and litigation. Each method offers different advantages depending on the nature of the dispute. Negotiation and mediation emphasize collaboration to reach an agreement, while arbitration and litigation involve third-party decisions. Understanding these options can empower you to choose the best path forward in your Molina Healthcare Provider Dispute Resolution Request.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


