Get Envisionrxoptions Prior Authorization Request Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the EnvisionRxOptions Prior Authorization Request Form online
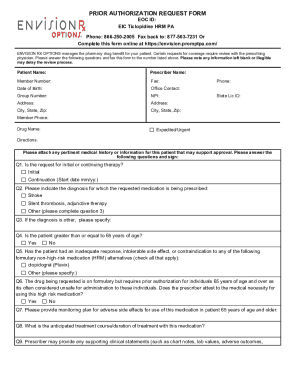
Properly completing the EnvisionRxOptions Prior Authorization Request Form is essential for securing necessary coverage for patients' medications. This guide offers a detailed, step-by-step approach to filling out the form online, ensuring clarity and ease of use for all individuals involved.
Follow the steps to accurately complete the form.
- Press the ‘Get Form’ button to access the Prior Authorization Request Form and open it for completion.
- Enter the patient's information including their name, date of birth, member number, and phone number in the designated fields.
- Provide the prescriber's details including their name, contact number, NPI (National Provider Identifier), and state license ID to ensure proper identification.
- Fill out the group number and the office contact person's information to facilitate communication.
- Indicate if the request is expedited or urgent by checking the appropriate box.
- Detail the medication information by entering the drug name and directions for use in the specified areas.
- Attach any relevant medical history or additional information that may support the authorization request.
- Answer the questions regarding the patient's diagnosis, providing a unique peer-reviewed journal article for medical necessity reviews if required.
- Include any supporting clinical statements such as lab values or treatment failures to strengthen the request for a formulary exception.
- Have the prescriber sign and date the form to validate the request.
- Review all entered information for accuracy, save the changes, and choose to download, print, or share the completed form as needed.
Complete the EnvisionRxOptions Prior Authorization Request Form online to support your patient's medication needs.
Related links form
Responsibility for obtaining preauthorization often resides with the healthcare provider, but patients can also take action. By utilizing the EnvisionRxOptions Prior Authorization Request Form, you can facilitate this process independently if needed. It's essential to stay engaged and communicate with your provider to ensure all necessary documents are submitted promptly. This proactive approach can speed up access to your required medications.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


