Get Aetna - Medical Exception/prior Authorization/precertification Request For Prescription
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Aetna - Medical Exception/Prior Authorization/Precertification Request For Prescription online
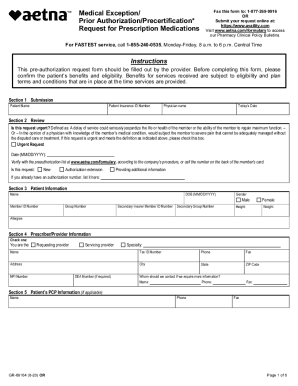
Filling out the Aetna Medical Exception/Prior Authorization/Precertification Request for Prescription form online is an essential step in ensuring that patients receive the necessary medications and treatments. This guide provides clear and detailed instructions for each section of the form, enabling users to complete it efficiently.
Follow the steps to successfully complete the online form.
- Press the ‘Get Form’ button to access the form and open it in your preferred editor.
- In Section 1, Submission, enter the patient’s name and insurance ID number. Include the physician’s name and today’s date.
- In Section 2, Review, indicate if this request is urgent by checking the appropriate box. Provide the date and select whether this request is for new authorization, an extension, or additional information. If applicable, include the existing authorization number.
- Section 3, Patient Information, requires the patient's name, date of birth, gender, member ID number, group number, secondary insurance member ID, secondary group number, height, weight, and any allergies.
- In Section 4, Prescriber/Provider Information, specify if you are the requesting or servicing provider. Fill in your specialty, name, tax ID number, phone, fax, address, city, state, ZIP code, NPI number, and DEA number if required.
- Section 5 asks for the patient's primary care provider's information, if applicable. Input their name and contact details.
- In Section 6, Medication/Medical & Dispensing Information, specify whether it's a new therapy or renewal, the route of administration, medication name, dose/strength, frequency, length of therapy, number of refills, and quantity. List previous drugs tried with their dosage.
- Section 7 requires justification for the requested medication. Include medical rationale, chart notes, and why alternative options are not acceptable.
- In Section 8, input all relevant ICD codes and their descriptions. Summary of diagnosis helps expedite the processing of your request.
- Review all sections for accuracy and completeness. Once finalized, save your changes, and you can choose to download, print, or share the form.
Complete your documents online today for efficient processing!
What is a Prior Authorization? A prior authorization (PA), sometimes referred to as a “pre-authorization,” is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine, medical device or procedure.
Fill Aetna - Medical Exception/Prior Authorization/Precertification Request For Prescription
Request for Prescription. Medications. See our precertification lists or utilize our CPT code lookup to see whether a procedure or service requires prior approval. Discover the Aetna difference. To initiate a request, submit electronically on Availity or call our. Precertification Department. Before completing this form, please confirm the patient's benefits and eligibility.
Industry-leading security and compliance
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


