Loading
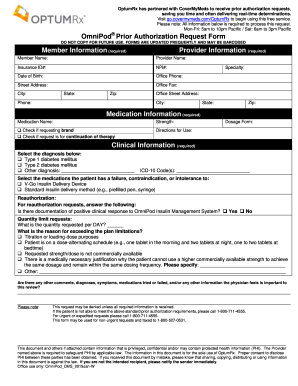
Get Omnipod Prior Authorization Request Form Member ...
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the OmniPod Prior Authorization Request Form Member online
Filling out the OmniPod Prior Authorization Request Form is a crucial step in obtaining necessary medication coverage. This guide will walk you through the process of completing the form online, ensuring that all required information is provided accurately and effectively.
Follow the steps to complete the form online.
- Press the ‘Get Form’ button to access the OmniPod Prior Authorization Request Form. This will open the form in your editor for filling out.
- Enter the member information in the required fields, including the member's name, date of birth, insurance ID number, and contact information.
- Provide the provider information by filling out the provider's name, NPI number, office phone, and address.
- Move to the medication information section and enter the medication name, strength, and check the relevant boxes for brand requests or continuation of therapy.
- In the clinical information section, select the appropriate diagnosis for the patient, and fill in the ICD-10 code.
- Indicate any medications the patient has had failure, contraindication, or intolerance to, by checking the relevant options.
- If this is a reauthorization request, answer the question regarding the documentation of a positive clinical response to the OmniPod system.
- Input the requested daily quantity and the reason for exceeding plan limitations, providing necessary details as prompted.
- Include any additional comments or pertinent information the physician deems significant for this review.
- Review the completed form, ensuring all sections are filled out completely and accurately. You can now save changes, download, print, or share the form as needed.
Complete your OmniPod prior authorization request today to ensure timely access to your medication.
For urgent or expedited requests please call 1-855-297-2870. This form may be used for non-urgent requests and faxed to 1-844-403-1029. OptumRx has partnered with CoverMyMeds to receive prior authorization requests, saving you time and often delivering real-time determinations.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


