Loading
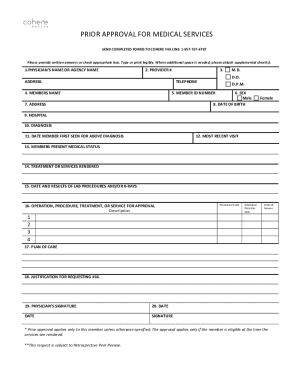
Get Cohere Health Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Cohere Health Prior Authorization Form online
Filling out the Cohere Health Prior Authorization Form online can streamline your request for medical services. This guide provides step-by-step instructions on how to accurately complete each section of the form to ensure a smooth submission process.
Follow the steps to complete the form efficiently.
- Press the ‘Get Form’ button to access the form and open it for completion.
- Begin by entering the physician's name or the agency name in the designated field. Ensure this information is clear to facilitate communication.
- Input the provider number next to the agency name, followed by the complete address to ensure accurate identification of the service provider.
- Fill in the physician's date of birth and telephone number to provide contact information for any follow-up inquiries.
- Next, enter the member’s name and member ID number to identify the individual for whom the authorization is being requested.
- Select the member's sex by marking the appropriate box and include the member's date of birth to confirm eligibility.
- Provide the member's address for additional reference, which will aid in verifying the member’s details.
- Indicate the hospital where the member is receiving treatment. This clarifies the location of services provided.
- In the diagnosis section, provide the relevant medical diagnosis, ensuring to date when the member was first seen for this condition.
- Document the date of the member's most recent visit related to their medical status, which gives context about the current health condition.
- Describe the member’s current medical status in detail to provide insights into ongoing treatment needs.
- Outline the treatment or services rendered thus far to substantiate the authorization request.
- Indicate the date and results of any lab procedures or x-rays that are relevant to the diagnosis.
- For the approval request, list the operation, procedure, treatment, or service required, including a description, procedure code, estimated price per unit, and number of units needed.
- Summarize the plan of care that outlines the intended treatment approach and justification for the requested services.
- Sign and date the form, confirming the accuracy of the information provided before submission.
- Once completed, save the changes, download the form, print it, or share it as needed.
Submit the completed forms online to ensure a timely review of your request.
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


