Loading
Get Prior Authorization Form (drugs Administered In Office ...
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Prior Authorization Form (Drugs Administered In Office) online
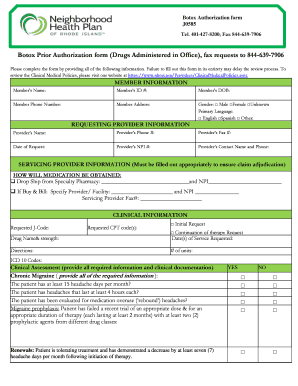
Completing the Prior Authorization Form for drugs administered in office can be a critical step in ensuring patients receive the necessary treatments. This guide provides clear and detailed instructions on how to accurately fill out the form online.
Follow the steps to successfully complete the prior authorization form.
- Click the ‘Get Form’ button to obtain the form and open it for editing.
- Begin by filling in the member information section, which includes the member’s name, ID number, date of birth, phone number, address, gender, and primary language.
- Next, provide the requesting provider's information, including their name, phone number, fax number, date of request, NPI number, and contact name and phone.
- Fill out the servicing provider's information. Specify how the medication will be obtained by selecting either 'Drop Ship from Specialty Pharmacy' or 'Buy & Bill' and providing relevant details accordingly.
- In the clinical information section, enter the requested J-Code and CPT code(s). Indicate whether this is an initial request or a continuation of therapy. Include the drug name and strength, date(s) of service requested, directions for use, number of units, and any applicable ICD-10 codes.
- Complete the clinical assessment by addressing the specific questions related to chronic migraine, hyperhidrosis, overactive bladder, or other conditions as applicable. Ensure all required information and clinical documentation are provided.
- Finally, ensure the form is signed by the requesting provider and enter the date of signature. Review the completed form for accuracy and completeness.
- After reviewing, save changes, download, print, or share the form as needed.
Complete your documents online now to ensure timely processing.
These steps are usually done manually, often through a cascade of phone calls, faxes and emails between payer and provider. The responsibility falls on the provider to continue to follow up with the insurance company until there is resolution of the prior authorization request — an approval, redirection, or denial.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


