Loading
Get Optumrx Emgality Prior Authorization Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Optumrx Emgality Prior Authorization Form online
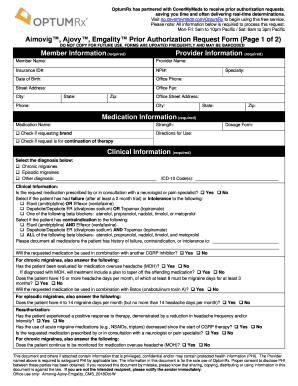
Filling out the Optumrx Emgality Prior Authorization Form online can be a straightforward process if you understand the required components. This guide provides clear and comprehensive instructions for each section of the form, making it easier for users to submit their requests accurately and efficiently.
Follow the steps to complete the form successfully.
- Press the ‘Get Form’ button to obtain the form and open it in your preferred online editing tool.
- Begin by entering the member information, including the member name, insurance ID number, date of birth, and their contact details.
- In the provider information section, input the provider name, office phone, fax number, address, and specialty.
- For medication information, include the medication name, strength, and specify if you are requesting the brand version. Provide directions for use and the dosage form.
- In the clinical information section, select the diagnosis related to the request. If applicable, please fill in the ICD-10 codes.
- Indicate whether the medication has been prescribed by or consulted with a neurologist or pain specialist.
- Check any previous medications the patient has tried, documenting any failures, contraindications, or intolerances.
- For chronic migraines, answer additional questions regarding diagnostic evaluations for medication overuse headache and treatment plans.
- Fill out the section pertaining to quantity limits, stating the amount requested per month and the justification for any exceeding quantity.
- Lastly, review all entries for accuracy and completeness before saving, downloading, printing, or sharing the form as needed.
Complete your documents online today for a streamlined experience.
Typically, within 5-10 business days of receiving the prior authorization request, your insurance company will either: Approve your request. Deny your request. Ask for more information.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


