Loading
Get Allwell Reconsideration Form
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Allwell Reconsideration Form online
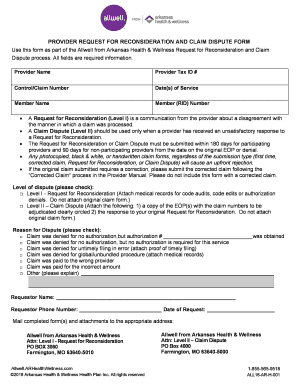
Completing the Allwell Reconsideration Form is essential for addressing disagreements regarding claim processing. This guide provides a clear, step-by-step approach to help you fill out the form accurately and effectively online.
Follow the steps to fill out the Allwell Reconsideration Form online.
- Press the ‘Get Form’ button to obtain the Allwell Reconsideration Form and open it in your document editor.
- In the first section, input the provider name and provider tax identification number (Tax ID #). These details help identify the submitting entity.
- Next, enter the control or claim number associated with the claim in question. This information assists in tracking the claim.
- Fill in the date or dates of service related to the claim being reconsidered or disputed. Accurate dates are crucial for the process.
- Provide the member's name and their Member (RID) number, ensuring correct identification of the individual involved.
- Indicate the level of dispute. Select either Level I - Request for Reconsideration or Level II - Claim Dispute based on your situation.
- For Level I, attach any relevant medical records if applicable. If filing a Level II dispute, ensure to include a copy of the Explanation of Payment (EOP) and your original Request for Reconsideration response.
- Select the reason for the dispute by checking the appropriate box. If your reason is not listed, choose 'Other' and provide a brief explanation.
- Lastly, fill in your name, phone number, and the date of the request. This personal information is essential for follow-up communication.
- Once all fields are completed, review your form for accuracy. You can then save changes, download, print, or share the final document.
Complete your Allwell Reconsideration Form online today to ensure your claims are processed correctly.
If you disagree with an action taken by your Medi-Cal managed care plan, you generally must first file an appeal with your managed care plan. You have 60 calendar days from the date of the notice of action to file an appeal with the managed care plan.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


