Loading
Get Psc Prior Authorization Form. Prior Authorization Form For .
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the PSC Prior Authorization Form online
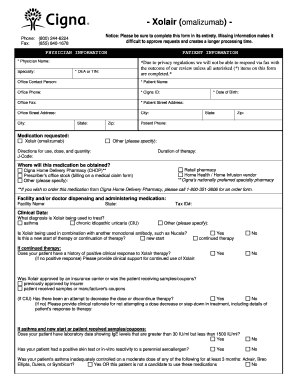
Completing the PSC Prior Authorization Form is crucial for obtaining approval for medication requests. This guide provides a clear and supportive walkthrough of each section of the form to ensure that users can fill it out accurately and efficiently.
Follow the steps to complete the form successfully
- Click the ‘Get Form’ button to access the PSC Prior Authorization Form and open it in your browser.
- Fill in the physician information, including the physician's name, specialty, DEA or TIN, and office contact person. Ensure all fields marked with an asterisk (*) are completed to avoid delays.
- Provide the patient information, such as the patient's name, Cigna ID, address, date of birth, and contact number. Accurate information is essential for processing.
- Specify the medication requested, including any additional details on directions for use, dosage, and quantity needed.
- Indicate where the medication will be obtained by selecting one of the options provided, such as a retail pharmacy or Cigna Home Delivery Pharmacy.
- Complete the clinical data section by providing the reason for the medication request, including relevant medical history and previous treatments. Make sure to provide comprehensive information to support the request.
- If applicable, document any attempts to reduce dosage or discontinue therapy and include clinical rationale for the patient's ongoing need for the medication.
- Once all sections are filled out, review the form for accuracy. Ensure all required fields are completed to facilitate timely processing.
- Save the form changes, and you may choose to download, print, or share it according to your needs.
Complete and submit your PSC Prior Authorization Form online today to streamline your medication approval process.
Prior authorization (also called “preauthorization” and “precertification”) refers to a requirement by health plans for patients to obtain approval of a health care service or medication before the care is provided. This allows the plan to evaluate whether care is medically necessary and otherwise covered.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


