Loading
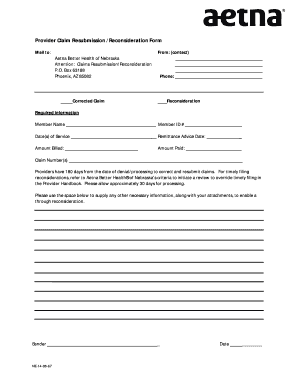
Get Provider Claim Resubmission /reconsideration Form Mail To: Aetna Better Health Of Nebraska
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Provider Claim Resubmission /Reconsideration Form Mail To: Aetna Better Health Of Nebraska online
Filling out the Provider Claim Resubmission /Reconsideration Form is crucial for healthcare providers seeking to correct and resubmit claims efficiently. This guide will walk you through each component of the form to ensure you provide all necessary information accurately.
Follow the steps to complete the form successfully.
- Press the ‘Get Form’ button to obtain the form and open it in your preferred editing tool.
- Begin by entering your contact information in the 'From:' section, which includes your name and phone number.
- Indicate whether you are submitting a corrected claim or a reconsideration by filling in the relevant section.
- Fill in the 'Required Information' section with the member's name, date(s) of service, amount billed, member ID number, remittance advice date, and amount paid.
- Enter the claim number(s) associated with the submission, ensuring accuracy to avoid processing delays.
- Use the space provided for any additional necessary information, including notes or explanations that could support your claim.
- Review your form for completeness and accuracy, then save changes to your document.
- Finally, download, print, or share the completed form as required for submission.
Complete the Provider Claim Resubmission /Reconsideration Form online to ensure a smooth and efficient claims process.
Call Member Services at 1-800-279-1878 (TTY: 711) and choose the crisis option. We're here for you 24 hours a day, 7 days a week.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


