Loading
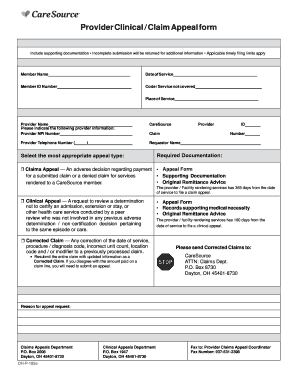
Get Provider Clinical / Claim Appeal Form Please Note The Following To Avoid Delays In Processing
How it works
-
Open form follow the instructions
-
Easily sign the form with your finger
-
Send filled & signed form or save
How to fill out the Provider Clinical / Claim Appeal Form to avoid delays in processing online
Filling out the Provider Clinical / Claim Appeal Form accurately is essential to ensure timely processing of your clinical or claims appeals. This guide provides clear, step-by-step instructions to help you navigate the form effectively and avoid common pitfalls.
Follow the steps to successfully complete the Provider Clinical / Claim Appeal Form.
- Click ‘Get Form’ button to access the Provider Clinical / Claim Appeal Form directly in your browser.
- Begin by providing the patient information. Fill out the following fields: Member Name, Date of Service, Member ID Number, Code/Service Not Covered, Place of Service, and Provider Name.
- Next, complete the provider information section. Enter the Provider NPI Number, Provider Telephone Number, and Requestor Name.
- Select the most appropriate appeal type from the options provided: Claims Appeal, Clinical Appeal, or Corrected Claim. Each option has specific documentation requirements, which you must follow.
- Depending on the appeal type selected, gather the required documentation. For Claims Appeal, include the Appeal Form, Supporting Documentation, and Original Remittance Advice. For Clinical Appeal, submit the Appeal Form, Records supporting medical necessity, and Original Remittance Advice.
- Clearly state the reason for your appeal request in the designated section to provide context to the reviewer.
- After completing the form and attaching all necessary documentation, you can save your changes, download the completed form, print it for mailing, or share it as needed.
Ensure all required fields are filled and documentation is attached before submitting your appeal online.
You have 1 year from the date of occurrence to file an appeal with the NHP. You will receive a decision in writing within 60 calendar days from the date we receive your appeal.
Industry-leading security and compliance
US Legal Forms protects your data by complying with industry-specific security standards.
-
In businnes since 199725+ years providing professional legal documents.
-
Accredited businessGuarantees that a business meets BBB accreditation standards in the US and Canada.
-
Secured by BraintreeValidated Level 1 PCI DSS compliant payment gateway that accepts most major credit and debit card brands from across the globe.


